WHO CNS5 Classification: What It Means for Neurological Diagnoses and Treatment
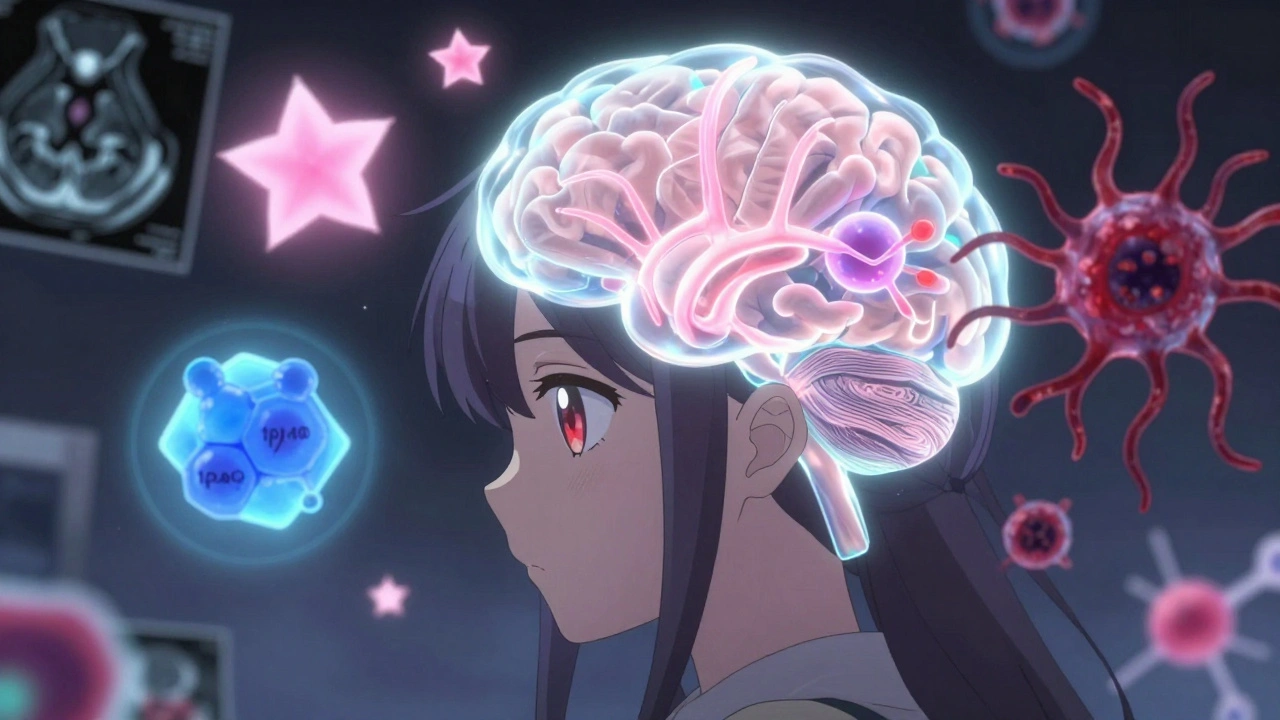
When doctors diagnose a brain tumor or other central nervous system disorder, they rely on a global standard called the WHO CNS5 classification, the fifth edition of the World Health Organization’s system for classifying tumors of the brain and spinal cord. Also known as CNS5, it’s the most up-to-date guide used by pathologists, neurologists, and oncologists worldwide to define what a tumor is, how aggressive it is, and how it should be treated. This isn’t just a list of names—it’s a living framework that ties molecular biology to real-world outcomes. Before CNS5, tumors were labeled mostly by how they looked under a microscope. Now, they’re defined by their genetic fingerprints, which changes everything about prognosis and therapy.
The WHO CNS5 classification, the fifth edition of the World Health Organization’s system for classifying tumors of the brain and spinal cord. Also known as CNS5, it’s the most up-to-date guide used by pathologists, neurologists, and oncologists worldwide to define what a tumor is, how aggressive it is, and how it should be treated. isn’t just about tumors. It reshapes how we understand conditions like gliomas, meningiomas, and even rare pediatric brain cancers. For example, a tumor once called a "low-grade glioma" might now be classified as an IDH-mutant astrocytoma with a specific mutation profile—something that directly affects whether a patient gets chemotherapy, radiation, or just monitoring. This shift means two patients with tumors that look identical under a microscope can have completely different treatment paths because of their DNA. The classification also recognizes that some tumors once thought to be benign can behave aggressively if they carry certain genetic markers, and others once seen as deadly can be managed long-term with targeted drugs.
What makes CNS5 different from earlier versions is how deeply it integrates lab data into diagnosis. It doesn’t just say "this is a grade 2 tumor." It says "this is a grade 2 IDH-mutant astrocytoma with 1p/19q co-deletion," which tells doctors not just what it is, but how it will likely behave and respond to treatment. This level of detail helps avoid overtreating some patients and under-treating others. It also means clinical trials can now be designed around specific molecular subtypes instead of broad categories, leading to more effective therapies. For patients, this translates into more personalized care—less guesswork, fewer side effects from unnecessary treatments, and better chances of long-term control.
Behind the scenes, this system is driven by global collaboration. Labs from the U.S., Europe, Asia, and beyond share data to refine categories, validate biomarkers, and update definitions. It’s not static—new subtypes are added every few years as research uncovers more about tumor biology. That’s why a diagnosis made in 2023 might be interpreted differently than one from 2019. If you or a loved one received a neurological diagnosis recently, chances are it was based on CNS5. And if you’re comparing treatment options or second opinions, knowing this system exists helps you ask better questions: "What’s the molecular profile?" "Which subtype does this fall under?" "How does that change my prognosis?"
Below, you’ll find real-world articles that connect directly to how this classification affects patients, doctors, and drug development—from how generics are chosen for CNS-related conditions to how side effects are tracked after new treatments are approved. These aren’t just medical updates—they’re stories of how science is making neurological care more precise, safer, and more human.
Brain Tumors: Types, Grades, and Multimodal Treatments Explained
Understand brain tumor types, grades, and modern treatments based on the latest WHO CNS5 guidelines. Learn how molecular testing changes survival outcomes and what new therapies like vorasidenib offer in 2025.
View More