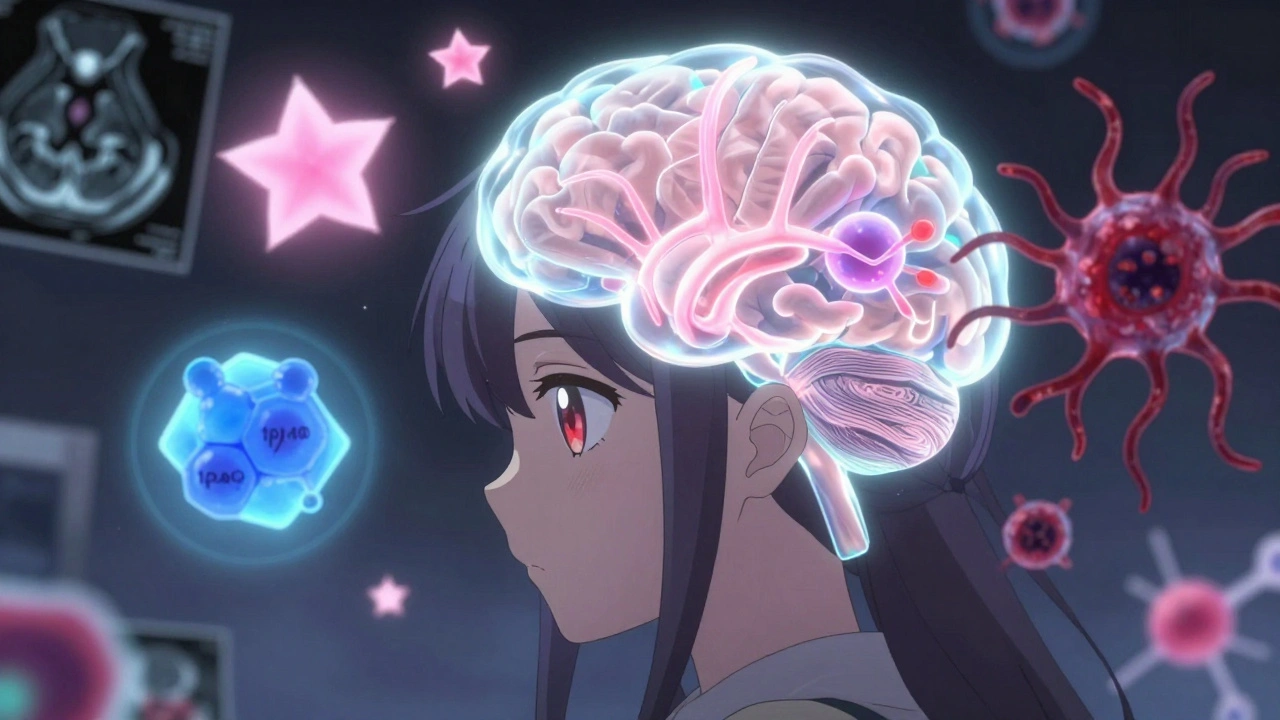
Multimodal Brain Tumor Treatment: Combining Surgery, Radiation, and Drugs for Better Outcomes
When it comes to multimodal brain tumor treatment, a coordinated approach using surgery, radiation, and drug therapies to attack brain tumors from multiple angles. Also known as combination therapy, it’s become the standard because single treatments rarely stop aggressive tumors from coming back. This isn’t just theory—it’s what doctors use every day in hospitals across the country to give patients the best shot at living longer and feeling better.
One key part of this strategy is brain tumor surgery, the removal of as much tumor tissue as possible without damaging healthy brain areas. It’s often the first step, especially when the tumor is accessible. But surgery alone isn’t enough. Even if the surgeon removes 99% of the tumor, leftover cells can grow back. That’s why radiation therapy for brain tumors, high-energy beams aimed precisely at the tumor site to kill remaining cancer cells follows. Modern techniques like stereotactic radiosurgery let doctors target small areas with minimal harm to surrounding tissue, something you won’t find in older treatment plans.
Then there’s chemotherapy brain tumors, drugs that travel through the bloodstream to destroy cancer cells anywhere in the body. Not all chemo works on brain tumors—the blood-brain barrier blocks many drugs. But newer agents like temozolomide cross that barrier and are now routine after surgery and radiation. And it’s not just traditional chemo anymore. targeted brain cancer therapy, medicines designed to attack specific genetic mutations in tumor cells is changing the game for patients with certain tumor types, like those with IDH or EGFR mutations. These treatments are more precise, often with fewer side effects than older chemo.
What makes multimodal treatment work isn’t just the tools—it’s how they’re timed and layered. Surgery reduces the tumor bulk, radiation cleans up the edges, and drugs hunt down the invisible spread. Patients don’t get all of this at once. It’s a sequence, sometimes stretching over months. And it’s not one-size-fits-all. A young patient with a fast-growing glioblastoma gets a different mix than an older adult with a slow-growing meningioma.
You’ll see in the articles below how this approach connects to real-world issues: how drug costs affect access to targeted therapies, why generic versions of chemo drugs matter for long-term care, how side effects from radiation are managed, and what patients should track when switching treatments. These aren’t abstract concepts—they’re daily decisions that shape survival and quality of life. Whether you’re a patient, caregiver, or just trying to understand what’s happening, the posts here give you the practical details you need—no jargon, no fluff, just what works and why.
Brain Tumors: Types, Grades, and Multimodal Treatments Explained
Understand brain tumor types, grades, and modern treatments based on the latest WHO CNS5 guidelines. Learn how molecular testing changes survival outcomes and what new therapies like vorasidenib offer in 2025.
View More