Glioblastoma: What It Is, How It’s Treated, and What You Need to Know
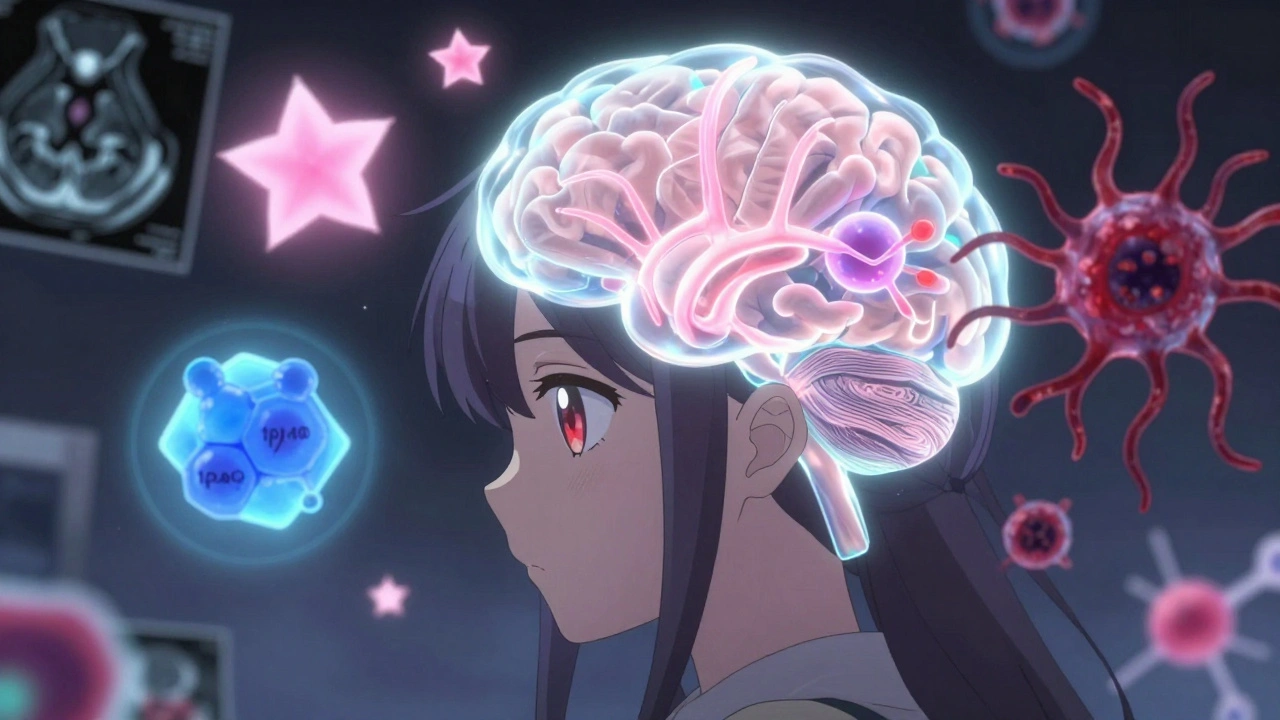
When someone is diagnosed with glioblastoma, a fast-growing, aggressive type of brain tumor that starts in glial cells. Also known as grade IV astrocytoma, it’s the most common and deadly primary brain cancer in adults. Unlike slower-growing tumors, glioblastoma spreads quickly through brain tissue, making complete removal nearly impossible. It doesn’t usually spread outside the brain, but inside, it’s relentless.
Most people with glioblastoma are treated with a mix of surgery, the first step to remove as much of the tumor as safely possible, followed by radiation therapy, high-energy beams aimed at the tumor site to kill remaining cells, and chemotherapy, usually with temozolomide, taken daily during and after radiation. These aren’t cures—they’re ways to slow the tumor down and give more time. Survival rates are low: about half of patients live less than 15 months after diagnosis. But some live longer, especially if the tumor has a specific genetic marker called MGMT methylation, which makes it more responsive to chemo.
There’s no one-size-fits-all approach. Age, overall health, and how much of the tumor can be removed during surgery all affect outcomes. Younger patients with fewer symptoms and complete resection tend to do better. New treatments—like tumor-treating fields (a wearable device that uses electric fields to disrupt cancer cell division) and immunotherapy trials—are being tested, but most are still experimental. What’s clear is that treatment isn’t just about drugs or scans. It’s about managing side effects like fatigue, memory loss, and seizures, which can be just as hard to live with as the tumor itself.
Many people with glioblastoma end up taking multiple medications at once—steroids to reduce swelling, anti-seizure drugs, pain relievers, and sometimes supplements. That’s where things get tricky. A drug that helps one symptom might interfere with another treatment. For example, some herbal supplements can affect how chemo works, and mixing pain meds with anti-seizure drugs can cause dangerous interactions. That’s why keeping a clear, updated medication list isn’t just helpful—it’s life-saving. You need to know exactly what you’re taking, why, and when, especially when switching between hospitals or specialists.
And while the science moves fast, the human side doesn’t. Families often struggle with how to talk about prognosis, when to stop aggressive treatment, and how to find comfort in the time left. Support groups, palliative care teams, and even simple tools like digital medication trackers can make a real difference—not in curing the disease, but in making the journey less chaotic. The posts below cover what actually matters: how to spot warning signs, how to ask the right questions at appointments, what side effects to report, and how to avoid dangerous drug mix-ups when you’re already overwhelmed. This isn’t about hope in the abstract. It’s about practical steps that help you stay in control when everything else feels out of it.
Brain Tumors: Types, Grades, and Multimodal Treatments Explained
Understand brain tumor types, grades, and modern treatments based on the latest WHO CNS5 guidelines. Learn how molecular testing changes survival outcomes and what new therapies like vorasidenib offer in 2025.
View More