Cystic Fibrosis: Practical Guide for Patients and Caregivers
Want straight, usable information about cystic fibrosis (CF)? This page gives plain answers on what CF is, how it affects lungs and digestion, key treatments you’ll hear about, and simple daily steps that really help.
What CF is and what to watch for
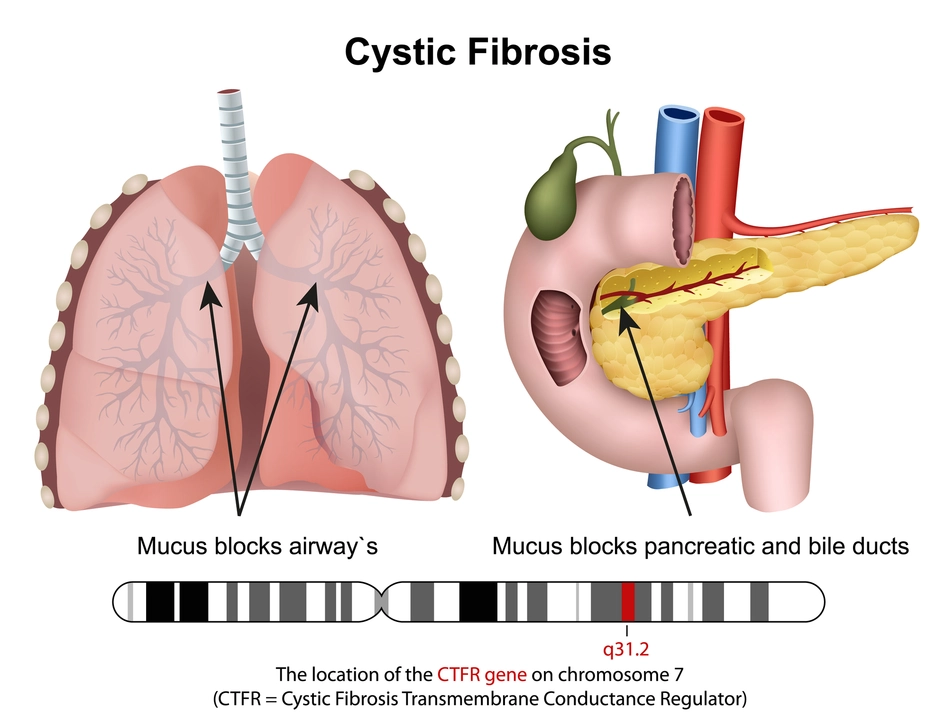
Cystic fibrosis is a genetic condition that makes mucus thick and sticky. That mucus clogs airways and traps germs, so people with CF get repeated lung infections and breathing problems. It also can stop enzymes from reaching the gut, making it hard to absorb food and gain weight. Common signs include persistent cough, frequent chest infections, poor growth, salty skin, and greasy stools. Newborn screening catches many cases early, but adults can be diagnosed later if symptoms show up.
Treatments doctors use right now
Treatment mixes medicines, airway care, nutrition, and infection control. CFTR modulators (drugs like ivacaftor and combination therapies) fix the underlying protein defect in many people and can dramatically improve lung function and weight. For airway clearance, people use chest physiotherapy, devices like vests, and inhaled treatments that thin mucus — for example, dornase alfa (Pulmozyme) or hypertonic saline. Inhaled antibiotics (such as tobramycin or aztreonam) target chronic infections from Pseudomonas and other bacteria. Pancreatic enzyme replacement helps digestion and nutrient absorption. And because CF increases risk of diabetes, regular blood sugar checks and diabetes care matter too.
Vaccines, hand hygiene, and avoiding crowded sick places reduce infection risk. When an infection flares, early antibiotics and clinic contact speed recovery and protect lung health.
Keep a log of lung symptoms, sputum colors, weight, and home spirometry numbers if you use them. Those simple records help your CF team spot problems early.
Daily habits that make a difference
Airway clearance every day keeps mucus moving. Exercise helps loosen secretions and boosts overall health. Eat calorie-dense meals and take enzymes with every bite. Try breathing techniques and relaxation — some people find Buteyko or paced breathing useful for symptom control. Don’t skip follow-ups: routine clinic visits, lung function tests, and sputum cultures guide treatment and catch issues early.
Mental health matters. Living with a chronic condition is draining, so reach out to counselors, support groups, or other people with CF for practical tips and emotional support.
Want deeper reading? Check our related articles on antibiotics and lung care like "10 Alternatives in 2025 to Minocycline," "7 Alternatives to Zithromax in 2025," "2024 Alternatives to Augmentin," and "Natural Asthma Relief: Best Breathing Techniques and Supplements." For CF-related diabetes, see our Glyset (miglitol) overview. These pieces explain medications, side effects, and safer choices when infections or diabetes complicate CF.
If you or a loved one has CF, connect with a specialized CF center. They’ll personalize treatments, teach airway techniques, and help coordinate nutrition and mental health care. Small daily steps add up — and the right team makes a big difference.
The Connection Between Cystic Fibrosis and Sinusitis
As someone who has researched the connection between cystic fibrosis and sinusitis, I've come to understand that these two conditions are closely related. Cystic fibrosis, a genetic disorder, causes the body to produce thick mucus, which often leads to chronic sinusitis. This is because the mucus clogs the sinus passages, creating the perfect environment for bacterial growth and infection. It's important for those with cystic fibrosis to work closely with their healthcare team to manage sinusitis and prevent complications. In conclusion, the relationship between cystic fibrosis and sinusitis highlights the importance of proper care and management to maintain the overall well-being of affected individuals.
View More