Understanding Cystic Fibrosis and Sinusitis
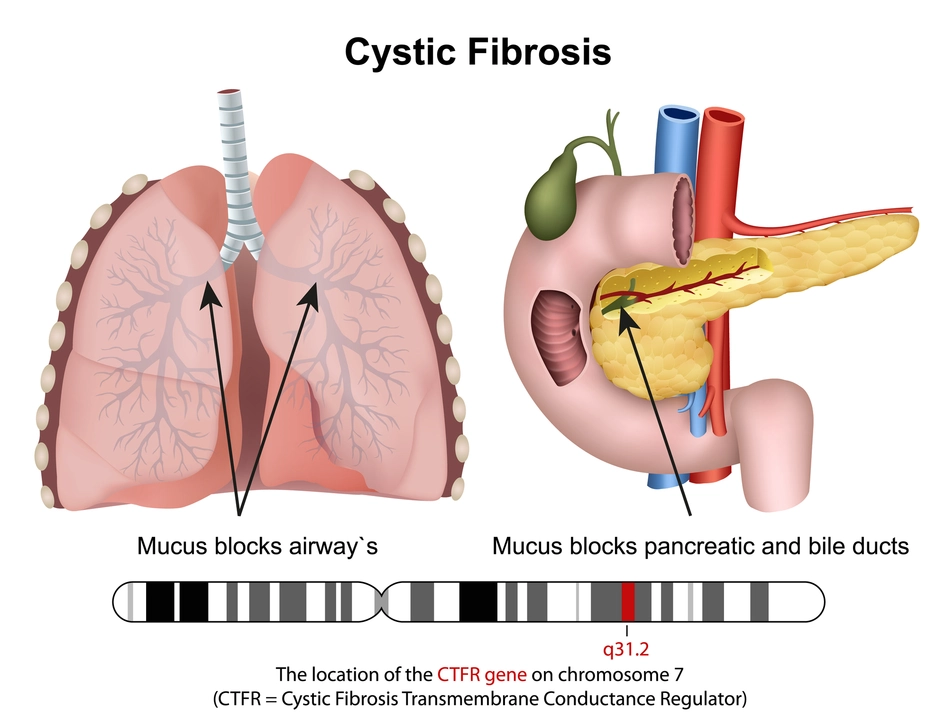
Before diving into the connection between cystic fibrosis and sinusitis, it's essential to understand these two medical conditions individually. Cystic fibrosis (CF) is a genetic disorder that affects the respiratory and digestive systems, causing thick and sticky mucus to build up in the lungs and other organs. This can lead to persistent lung infections and impaired breathing over time. Sinusitis, on the other hand, is an inflammation of the sinuses, typically caused by a bacterial, viral, or fungal infection. Symptoms include facial pain, congestion, and a runny nose.
The Role of Mucus in CF and Sinusitis
One of the primary connections between cystic fibrosis and sinusitis is the role that mucus plays in both conditions. In a healthy individual, mucus helps to trap and remove bacteria, viruses, and other harmful particles from the respiratory system. However, in individuals with CF, the mucus is thicker and stickier, making it more difficult for the body to clear away pathogens. This leads to an increased risk of infections, including sinusitis.
Moreover, the thick mucus in CF patients can block the sinus passages, making it difficult for the sinuses to drain properly. This creates a breeding ground for bacteria, leading to chronic sinusitis in many individuals with CF. In fact, studies have shown that more than 50% of people with CF experience sinusitis at some point in their lives.
Diagnosing Sinusitis in Individuals with CF
Diagnosing sinusitis in people with cystic fibrosis can be more challenging compared to those without CF. This is because many of the symptoms of sinusitis, such as coughing, nasal congestion, and difficulty breathing, are also typical symptoms of CF. Therefore, healthcare providers need to carefully evaluate the patient's history and perform additional tests to confirm a sinusitis diagnosis.
Some common diagnostic tests for sinusitis in CF patients include nasal endoscopy, sinus culture, and imaging studies such as X-rays, computed tomography (CT) scans, or magnetic resonance imaging (MRI). These tests help determine the extent of sinus inflammation and identify any potential complications, such as sinus polyps or a blockage in the sinus passages.
Treatment Options for Sinusitis in CF Patients
The treatment of sinusitis in individuals with cystic fibrosis often involves a combination of medical and surgical interventions. The primary goal of treatment is to reduce inflammation, clear mucus, and prevent further complications. Some common treatment options include:
1. Antibiotics: These medications are prescribed to target the specific bacteria causing the sinus infection. In CF patients, antibiotics may be given orally, intravenously, or through inhaled medications to ensure effective treatment.
2. Nasal irrigation: This involves flushing out the nasal passages with a saline solution to help clear mucus and reduce inflammation. Nasal irrigation can be done at home using a bulb syringe or a neti pot.
3. Mucus-thinning medications: These medications, such as hypertonic saline or dornase alfa, can help thin the mucus in the sinuses, making it easier for the body to clear away pathogens.
4. Sinus surgery: In some cases, surgery may be necessary to remove polyps or other obstructions in the sinus passages. This can help improve sinus drainage and reduce the risk of recurrent sinus infections.
Preventing Sinusitis in Individuals with Cystic Fibrosis
Preventing sinusitis in people with CF requires a proactive approach to managing their overall health. This includes maintaining a consistent daily routine that focuses on airway clearance, taking medications as prescribed, and attending regular medical appointments. Some additional prevention measures include:
1. Practicing good hygiene: Washing hands frequently and avoiding contact with individuals who are sick can help reduce the risk of catching a cold or other respiratory infection that could lead to sinusitis.
2. Using a humidifier: Keeping the air in your home moist can help thin mucus and make it easier for your body to clear away pathogens. Be sure to clean the humidifier regularly to prevent mold and bacteria growth.
3. Staying up-to-date on vaccinations: Ensuring that you receive all recommended vaccines, including the annual flu shot, can help protect against respiratory infections that may contribute to sinusitis.
By understanding the connection between cystic fibrosis and sinusitis, individuals with CF and their healthcare providers can work together to effectively manage and prevent sinus-related complications. This can ultimately help improve the overall quality of life for those living with this challenging genetic disorder.

Comments (17)
Linda Stephenson
Just dug into the link between cystic fibrosis and sinusitis and gotta say the mucus thing is a real nightmare. When the mucus gets super thick it literally plugs up the sinus passages and creates the perfect breeding ground for bugs. I found it crazy that over half of CF folks end up dealing with sinus infections at some point. The article does a solid job breaking down why the standard nose sprays often don’t cut it for them. Guess we all need to keep an eye on those airway‑clearing routines.
Sunthar Sinnathamby
Look, the medical world keeps tossing out half‑baked solutions while CF patients suffer. They slap on antibiotics and hope for the best, but the real issue is that sticky mucus – you can’t just mask it. If they spent half the effort on proper airway clearance, we’d see far fewer chronic sinus bouts.
Catherine Mihaljevic
They're hiding the truth about CF sinus treatments behind pharma profit motives
Michael AM
Good summary, especially the part about nasal irrigation – that’s a simple thing that actually helps. I’ve seen families use neti pots and notice less congestion. Also, reminding folks to keep their humidifiers clean is key, mold can make things worse. Keep the info coming, it’s super useful.
Rakesh Manchanda
The discourse presented elegantly intertwines pathophysiology with therapeutic stratagems, yet one might argue the epistemic rigor could be further refined. While the exposition on mucolytic agents is commendable, a deeper exploration of genotype‑specific responses would elevate the narrative. Moreover, the surgical considerations merit a more nuanced deliberation regarding postoperative outcomes. In sum, the article offers a commendable scaffold upon which future scholarly endeavors may build.
Erwin-Johannes Huber
Thanks for laying this out in a clear way. For anyone newly diagnosed, understanding the link between mucus viscosity and sinus blockage can be reassuring. It shows why sticking to routine chest physiotherapy matters beyond the lungs. Keep sharing these practical insights, they really make a difference.
Tim Moore
Esteemed readers, the correlation delineated herein between cystic fibrosis and sinusitis is both clinically pertinent and scientifically robust. The authors have judiciously cited pertinent literature to substantiate their claims, thereby enhancing the article’s credibility. It is imperative that clinicians assimilate these findings into holistic patient management protocols. Moreover, the discussion of adjunctive therapies such as hypertonic saline warrants further empirical investigation. I commend the comprehensive nature of this exposition.
Erica Ardali
Oh, the tragedy of thick, unforgiving mucus! It’s like a relentless tide engulfing the sinuses, a silent siege no one sees. The article paints a bleak yet honest portrait of the daily battle these patients endure. One can’t help but feel a pang of sorrow for every breath they fight for. Let’s hope the medical community rallies to break this vicious cycle.
Justyne Walsh
Well, isn’t it just typical that Western research keeps preaching generic solutions while ignoring our unique genetic backdrop. We should be demanding localized studies, not half‑baked global guidelines. It’s about time the Irish‑Celtic medical board steps up and says enough is enough.
Callum Smyth
Great rundown! 🎉 The practical tips on hygiene and humidifier use are spot‑on. Keep the community informed, it really helps families navigate daily challenges.
Xing yu Tao
Linda, your observations regarding mucus viscosity are well‑taken. Indeed, integrating consistent airway clearance with adjunctive therapies could mitigate sinus complications.
Adam Stewart
Sunthar, your critique highlights a critical need for better therapeutic strategies. A balanced approach might bridge the gap you’ve identified.
Selena Justin
Catherine, your caution about pharmaceutical influences is noted. Transparency in treatment efficacy remains paramount.
Bernard Lingcod
Michael, I echo your emphasis on nasal irrigation; it’s a low‑cost, high‑impact measure. Have you considered integrating sinus rinse schedules with physiotherapy sessions?
Raghav Suri
Rakesh, your call for genotype‑specific insights is spot on. Future studies should indeed parse those nuances for tailored interventions.
Freddy Torres
Erwin’s points underscore the value of routine care.
Andrew McKinnon
Alright, let’s unpack this whole CF‑sinus saga because the average Redditor deserves a deep dive. First off, the pathophysiology is simple in theory: mutant CFTR channels = dehydrated airway surface liquid. That dehydration translates to hyperviscous mucus that clogs not just bronchioles but also the ethmoidal air cells. When that plug sits there, you get a perfect anaerobic niche for Pseudomonas, Staph aureus, and a host of opportunists. Clinicians often throw broad‑spectrum antibiotics at the problem, but without addressing the rheology of the secretions, you’re just playing whack‑a‑mole. Enter mucolytics like dornase alfa, which enzymatically cleaves extracellular DNA, effectively thinning the sputum. But dornase isn’t a silver bullet for the sinuses; its delivery via nebulizer rarely reaches the maxillary cavities. That’s why some centers advocate for hypertonic saline sinus irrigations, leveraging osmotic gradients to draw water into the mucus. On the surgical front, functional endoscopic sinus surgery (FESS) can restore patency, yet post‑op restenosis rates remain non‑trivial. You’ve got to pair surgery with aggressive postoperative medical therapy, otherwise the benefits evaporate in weeks. From a preventive standpoint, daily chest physiotherapy, high‑frequency chest wall oscillation, and adherence to modulator therapies like ivacaftor dramatically reduce overall mucus load. Vaccination status is also crucial; influenza and pneumococcal vaccines blunt the seasonal surges that exacerbate sinus inflammation. Temperature‑controlled humidification can further modulate mucus viscosity, but remember to change the water daily to avoid biofilm formation. Psychologically, living with chronic sinusitis on top of CF can erode quality of life, so multidisciplinary care including mental health support is indispensable. Bottom line: a multimodal regimen-antibiotics, mucolytics, irrigation, possible surgery, and robust supportive care-offers the best shot at keeping those sinuses clear. Stay proactive, track your symptoms, and push your care team for personalized adjustments; complacency is the enemy.