Chronic Inflammation: What It Is and Why You Should Care
Have you had low-level aches, constant fatigue, or stubborn weight that won’t budge? Those can be signs of chronic inflammation — the long-term, low-grade immune activity that quietly wears down your body. Unlike sudden inflammation after an injury, chronic inflammation sticks around and raises the risk of heart disease, diabetes, arthritis and other problems.
How to recognize chronic inflammation
Look for persistent symptoms rather than a single bad day. Common clues are daily tiredness, waking stiff, unexplained joint pain, frequent minor infections, brain fog, and skin issues like psoriasis. You might also notice slow healing wounds or ongoing digestive trouble. A simple blood test for C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) can flag inflammation; your doctor may order those if symptoms add up.
Practical steps to lower inflammation now
Start with things you can control. Swap ultra-processed foods and sugary drinks for whole foods: vegetables, fruits, beans, nuts, whole grains and fatty fish. The Mediterranean-style mix — olive oil, veggies, fish and modest portions — consistently helps people reduce markers of inflammation.
Move more, but be smart. Aim for 30 minutes of moderate activity most days: brisk walking, cycling or swimming. Strength training twice weekly helps too. Exercise lowers inflammation, improves sleep, and helps lose belly fat, which fuels inflammation.
Manage stress with short daily practices. Five to ten minutes of focused breathing, a brief walk outside, or a consistent bedtime routine reduces stress hormones that drive inflammation. Sleep matters: aim for 7–9 hours. Even one or two nights of poor sleep raises inflammatory markers.
Simple supplements can help when diet falls short. Omega‑3 fish oil and vitamin D have good evidence for lowering inflammation in many people. Turmeric/curcumin may help too, but use standardized extracts and talk with your doctor, especially if you take blood thinners.
Quit smoking and limit alcohol. Smoking is a strong trigger for chronic inflammation. Alcohol in excess worsens inflammation and sleep quality; moderate intake or a break for a few weeks can show quick benefits.
If you have an obvious medical cause — like an autoimmune disease, chronic infection, or untreated sleep apnea — treating that condition is the most effective way to reduce inflammation. For autoimmune problems, doctors may recommend disease‑modifying drugs or biologics. Short courses of NSAIDs can ease symptoms but aren’t a long-term solution without a clear plan.
When to see a doctor: get checked if you have ongoing fever, rapid weight loss, severe joint swelling, or persistent symptoms that don’t respond to lifestyle changes. Bring a list of symptoms and any recent lab work. A primary care doctor can order CRP/ESR and guide you to a specialist if needed.
Small changes add up. Eating more plants, moving regularly, sleeping better and handling stress reduce inflammation for most people. If you’re unsure where to start, ask your doctor for a basic inflammation screen and a clear, step-by-step plan you can follow.
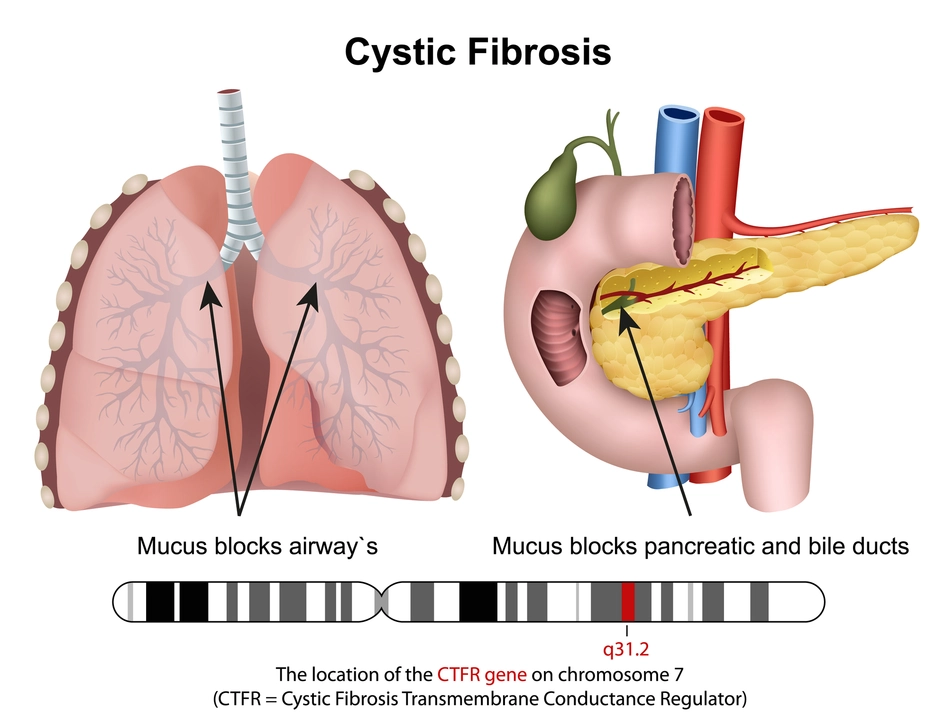
The Connection Between Cystic Fibrosis and Sinusitis
As someone who has researched the connection between cystic fibrosis and sinusitis, I've come to understand that these two conditions are closely related. Cystic fibrosis, a genetic disorder, causes the body to produce thick mucus, which often leads to chronic sinusitis. This is because the mucus clogs the sinus passages, creating the perfect environment for bacterial growth and infection. It's important for those with cystic fibrosis to work closely with their healthcare team to manage sinusitis and prevent complications. In conclusion, the relationship between cystic fibrosis and sinusitis highlights the importance of proper care and management to maintain the overall well-being of affected individuals.
View More