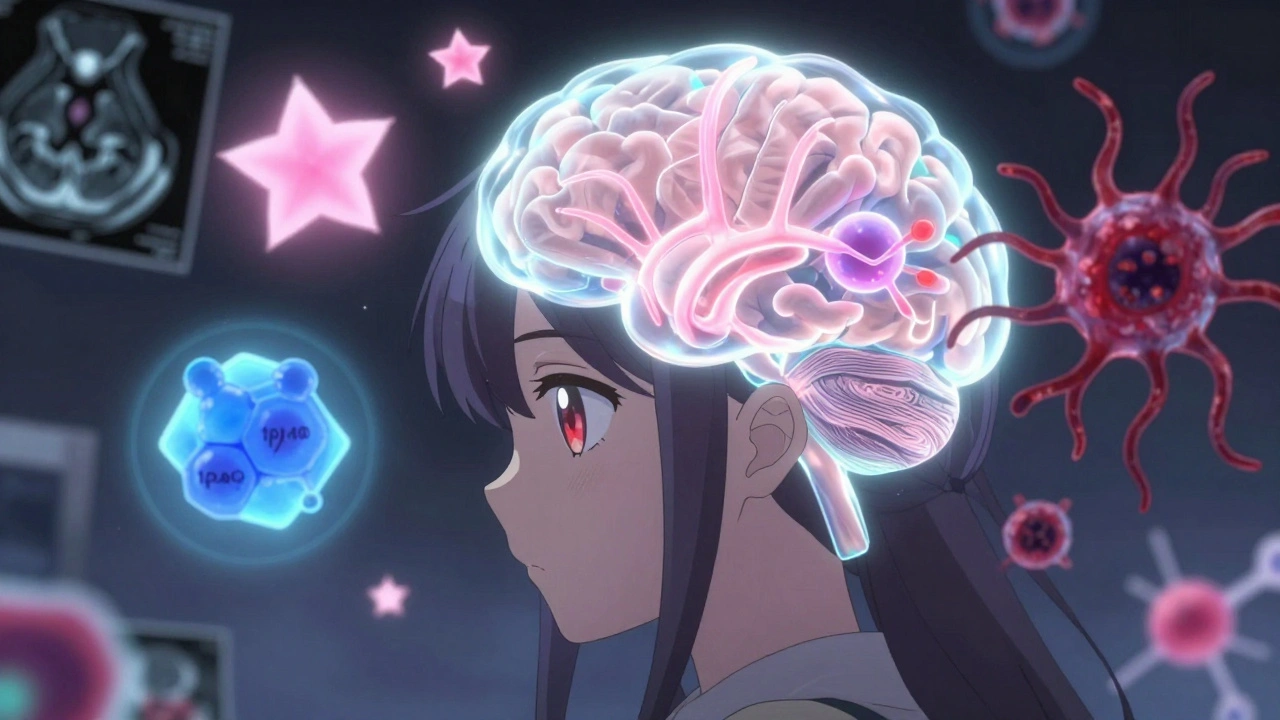
Brain Tumor Grades: What Each Level Means and How It Affects Treatment
When doctors talk about brain tumor grades, a system that classifies brain tumors by how abnormal the cells look and how fast they grow. Also known as tumor grading, it’s not just a label—it’s the foundation for every treatment decision. Unlike cancer staging, which looks at spread, grading focuses on the tumor’s behavior right where it is. A grade 1 tumor might grow slowly and be removable with surgery alone. A grade 4 tumor? It’s aggressive, spreads into nearby brain tissue, and needs a mix of surgery, radiation, and chemo.
The tumor grading system, a standardized scale from 1 to 4 used by neurologists and pathologists to assess brain tumors comes from the World Health Organization. Grade 1 tumors are the least aggressive—they look almost normal under the microscope and often don’t come back after removal. Grade 2 tumors are low-grade but can creep into healthy brain tissue, making complete removal tricky. Grade 3 tumors are malignant and grow faster; they’re often called anaplastic. And grade 4? That’s glioblastoma, the most aggressive type. It grows rapidly, resists treatment, and has a poor long-term outlook. These aren’t just numbers—they shape survival chances, treatment intensity, and even quality of life.
Knowing the grade helps answer the big questions: Will surgery be enough? Do I need radiation? Is chemo worth the side effects? A grade 1 meningioma might need no further treatment after removal. But a grade 4 glioblastoma requires a brutal, multi-month plan. The glioma classification, a subset of brain tumors that arise from glial cells and include most high-grade tumors is especially important here—most grade 3 and 4 tumors are gliomas. And while some tumors stay low-grade for years, others transform over time, which is why follow-up scans are non-negotiable.
What you won’t find in the grade is the full story. Two people with the same grade can have wildly different outcomes based on age, tumor location, genetic markers, and overall health. But the grade is the starting point. It tells you the enemy’s strength before you plan the battle. The posts below cover what you need to know next: how grades affect survival, why some tumors are harder to treat than others, how imaging and biopsies determine the grade, and what newer tests like molecular profiling are changing in the field. You’ll also find real talk about treatment side effects, what to ask your neuro-oncologist, and how to track changes over time. This isn’t theory—it’s what people actually face after a diagnosis.
Brain Tumors: Types, Grades, and Multimodal Treatments Explained
Understand brain tumor types, grades, and modern treatments based on the latest WHO CNS5 guidelines. Learn how molecular testing changes survival outcomes and what new therapies like vorasidenib offer in 2025.
View More