Beta-blockers: what they do and when they help
Beta-blockers are a group of medicines that slow your heart and reduce how hard it works. Doctors prescribe them for high blood pressure, angina (chest pain), some heart rhythm problems, heart failure, migraine prevention, and even performance anxiety. Some are taken as pills (metoprolol, atenolol, propranolol) and one common eye drop, timolol, treats glaucoma.
If you want the short version: they lower blood pressure and pulse, protect the heart after a heart attack, and can calm adrenaline-driven symptoms like shaking or fast heartbeat.
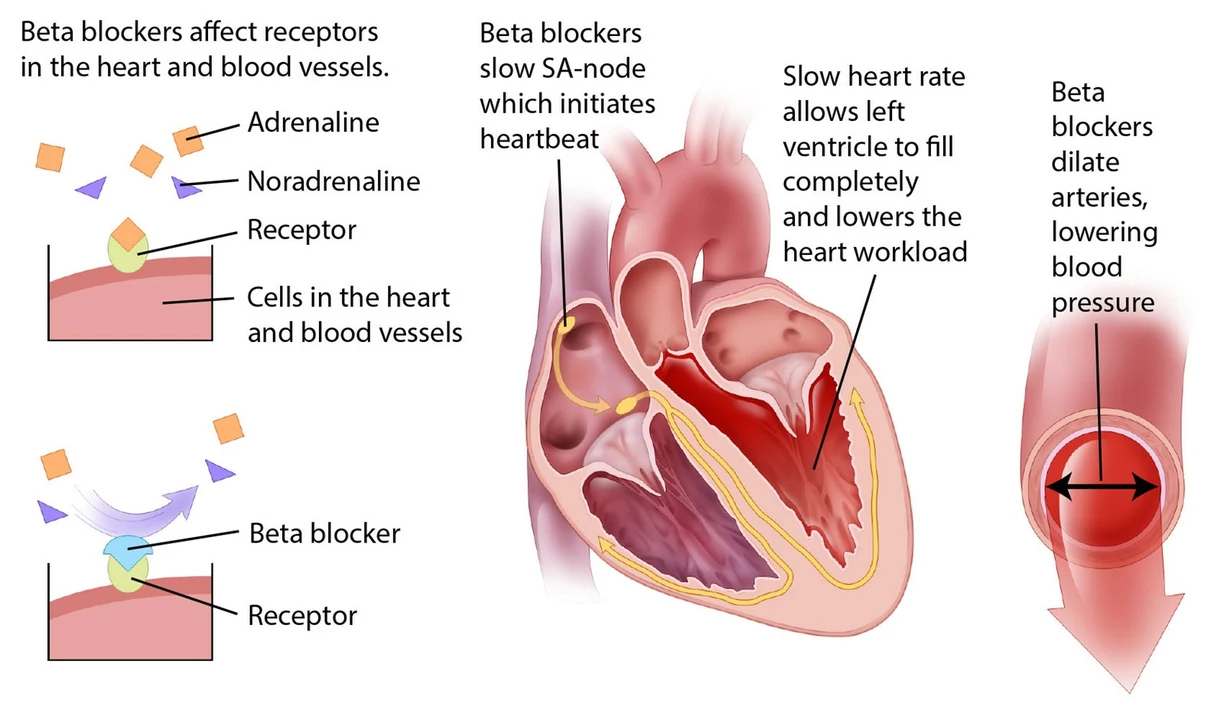
How they work and common examples
Beta-blockers block beta receptors that respond to adrenaline. That slows your heart rate and lowers blood pressure. Common oral names you’ll hear are metoprolol, propranolol, atenolol, bisoprolol, and nadolol. Timolol is used as an eye drop for glaucoma. Each drug has small differences — some are more selective for the heart, some last longer, and some cross into the brain more (which matters for anxiety or sleep effects).
What to expect and practical tips
When you start a beta-blocker you might feel tired, lightheaded, or cold hands and feet. Some people notice mild dizziness at first; that usually eases over a week or two. A common side effect is a slower heartbeat — that’s expected, but if your pulse drops under about 50 beats per minute or you feel faint, call your doctor. Other issues can include sleep changes, vivid dreams, or increased fatigue during exercise.
Don’t stop these drugs suddenly. Stopping abruptly can cause your blood pressure and heart rate to spike, and may trigger chest pain or worse in people with heart disease. If you need to stop, your doctor will taper the dose slowly.
Watch for interactions: combined use with some calcium channel blockers (like verapamil), certain antidepressants, or antiarrhythmics can dangerously slow the heart. If you take insulin or other diabetes drugs, beta-blockers can mask the typical warning signs of low blood sugar (like fast heartbeat). Always keep a current list of medicines and share it with your clinician.
Who should be cautious? If you have asthma or COPD with active wheeze, untreated low heart rate, or certain forms of heart block, beta-blockers may be risky. Still, selective beta-blockers are sometimes used cautiously under supervision. Pregnant or breastfeeding people should check with their provider about specific risks and alternatives.
Simple monitoring helps: check your blood pressure and pulse at home, report persistent dizziness or breathing problems, and attend follow-up visits for dose adjustments. If you’re preparing for surgery or need emergency care, tell providers you’re on a beta-blocker — it affects heart rate management during procedures.
Questions about which beta-blocker fits your situation? Talk to your doctor or pharmacist. They’ll match the drug, dose, and timing to your heart condition, other meds, and daily life so you get benefits with fewer side effects.
Antihypertensives: Beta-Blockers, ACE Inhibitors, and ARBs - What You Need to Know
Beta-blockers, ACE inhibitors, and ARBs are three key blood pressure medications with different uses, side effects, and benefits. Learn which is best for your condition and why some patients switch.
View MoreAtenolol vs. other beta-blockers: What sets it apart?
As a blogger, I've been researching the differences between Atenolol and other beta-blockers. What sets Atenolol apart is its selectivity for beta-1 receptors, which mainly affects the heart rather than other areas of the body. This makes it less likely to cause side effects like bronchoconstriction, which can be a problem with non-selective beta-blockers. Additionally, Atenolol has a longer half-life, meaning it can be taken once a day for better patient compliance. Overall, Atenolol appears to be a more targeted option with fewer side effects compared to other beta-blockers on the market.
View More