Understanding Beta-Blockers: An Introduction
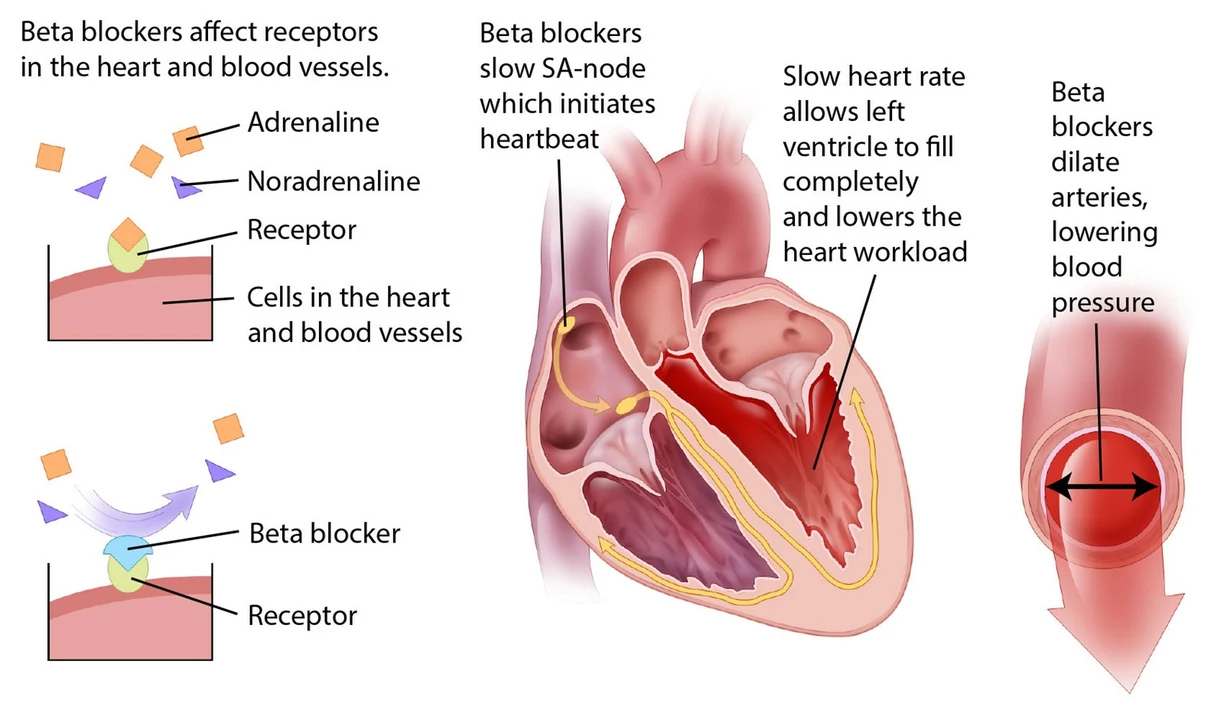
Beta-blockers are a group of medications that are commonly prescribed for a variety of cardiovascular conditions. They work by blocking the effects of stress hormones on the heart, helping to slow the heart rate and reduce blood pressure. In this article, we will focus on Atenolol, a popular beta-blocker, and compare it with other beta-blockers to understand what sets it apart.
Atenolol: A Closer Look
Atenolol is a selective beta-blocker, which means it specifically targets beta-1 receptors in the heart. This selectivity allows Atenolol to have a more focused effect on the heart, with fewer side effects on other organs and tissues. Atenolol is commonly prescribed for hypertension, angina, and as a preventive measure for heart attacks.
Propranolol: A Non-selective Beta-Blocker
Propranolol is another commonly prescribed beta-blocker, but unlike Atenolol, it is non-selective. This means that Propranolol targets both beta-1 and beta-2 receptors, causing a more widespread effect throughout the body. While this can be beneficial in some cases, such as treating migraines, it can also lead to more potential side effects.
Metoprolol: A Selective Beta-Blocker Similar to Atenolol
Metoprolol, like Atenolol, is a selective beta-blocker, targeting only beta-1 receptors. However, there are some differences between the two medications. Metoprolol has a shorter half-life than Atenolol, meaning it may need to be taken more frequently. Additionally, Metoprolol is available in an extended-release form, which can help to maintain consistent levels of the medication throughout the day.
Side Effect Profiles: Comparing Atenolol to Other Beta-Blockers
Because Atenolol is a selective beta-blocker, it tends to have fewer side effects than non-selective beta-blockers like Propranolol. Some common side effects of Atenolol include fatigue, dizziness, and cold hands and feet. However, these side effects are generally less severe and less common than those experienced by people taking non-selective beta-blockers.
Drug Interactions: What to Watch Out For
As with any medication, there is a potential for drug interactions when taking Atenolol. Some of the common medications that may interact with Atenolol include calcium channel blockers, antiarrhythmics, and certain antidepressants. It's essential to discuss all of your current medications with your doctor to ensure there are no harmful interactions.
Atenolol and Pregnancy: What You Need to Know
If you are pregnant or planning to become pregnant, it's essential to discuss your medications with your doctor. Atenolol has been classified as a pregnancy category D drug, which means there is evidence of potential harm to the fetus. However, your doctor may still prescribe Atenolol if the benefits outweigh the risks.
Dosage and Administration: How to Take Atenolol Safely
Atenolol is typically taken as a once-daily oral tablet, with the dosage determined by your doctor based on your specific needs and condition. It's essential to follow your doctor's instructions carefully and to never stop taking Atenolol without consulting your doctor, as this can lead to severe complications.
Atenolol vs. Other Beta-Blockers: Which One is Right for You?
Ultimately, the decision between Atenolol and other beta-blockers will depend on your individual needs, medical history, and the specific condition being treated. While Atenolol's selectivity and generally mild side effect profile make it an attractive option for many patients, other beta-blockers may be more appropriate in certain situations.
Conclusion: Understanding Your Options
In conclusion, Atenolol is a selective beta-blocker with several advantages over non-selective beta-blockers, including a more focused effect on the heart and fewer side effects. However, each individual's needs and medical history will play a significant role in determining the most appropriate beta-blocker for their situation. It's essential to have an open and honest conversation with your doctor about your options to ensure you receive the best possible care.

Comments (7)
Dheeraj Mehta
Atenolol’s cardioselectivity makes it a solid choice for patients with comorbid respiratory conditions :) Keeping side effects low is always a win.
Oliver Behr
The UK formulary prefers agents with shorter half‑lives for easier titration.
Tiffany W
The pharmacodynamic profile of atenolol is defined by its high β1‑adrenergic receptor affinity, which confers marked cardioselectivity. This selectivity reduces bronchoconstrictive risk in asthmatic patients, a crucial consideration in polypharmacy contexts. Moreover, atenolol exhibits a relatively low intrinsic sympathomimetic activity, thereby minimizing tachyphylaxis. Its hydrophilic nature limits central nervous system penetration, explaining the lower incidence of CNS‑related adverse effects compared with lipophilic counterparts. From a pharmacokinetic standpoint, the drug’s bioavailability approximates 50%, with an elimination half‑life of 6–9 hours, supporting once‑daily dosing schemas. Renal excretion predominates, rendering dosage adjustments essential in patients with impaired glomerular filtration. Clinical trials have demonstrated modest reductions in systolic blood pressure, typically in the range of 8–12 mmHg, when used as monotherapy. When combined with ACE inhibitors, the additive antihypertensive effect aligns with guideline‑directed therapy for high‑risk cohorts. However, comparative meta‑analyses indicate that atenolol does not confer superior mortality benefits relative to metoprolol or carvedilol in post‑myocardial infarction populations. Adverse effect profiling shows a predilection for fatigue and peripheral coldness, yet these are generally less severe than the bronchospasm risk associated with non‑selective agents. Drug–drug interaction potential is notable with concurrent calcium channel blockers, particularly verapamil, necessitating vigilant heart rate monitoring. Pregnancy category D classification underscores teratogenic concerns, warranting risk–benefit deliberation in gestational hypertension. Economic analyses reveal that generic atenolol remains among the most cost‑effective beta‑blockers in low‑resource settings. Nevertheless, patient adherence may be compromised by the perception of suboptimal efficacy, a psychosocial factor often omitted from efficacy endpoints. Future research should prioritize head‑to‑head trials incorporating quality‑of‑life metrics to elucidate true comparative advantage. In sum, atenolol’s mechanistic attributes render it a viable option, albeit one that must be contextualized within individual therapeutic goals.
Rajeshwar N.
Despite the mechanistic merits, recent meta‑analyses reveal no clear mortality advantage for atenolol over non‑selective beta‑blockers, and its peripheral side‑effects often compromise patient comfort. The data suggest that prescribers may be over‑valuing cardioselectivity at the expense of holistic outcomes.
Louis Antonio
Look, I’ve been on atenolol for years and the fatigue is real – you’re not fooling anyone with the “mild side‑effects” line. If you love feeling like a hamster on a wheel, go ahead, but most of us just want a drug that doesn’t make us feel dead.
Kyle Salisbury
In many South Asian clinics, cost considerations often tip the scale toward generic atenolol, even when clinicians recognize its pharmacologic limitations.
Angie Robinson
Your analysis misses the point entirely.