When your doctor orders a pulmonary function test, it’s not just another checkbox. It’s a window into how well your lungs are actually working-especially when you’re short of breath, coughing constantly, or just feel like you can’t catch your air. Two of the most important tests in this space are spirometry and DLCO. They’re simple, non-invasive, and surprisingly powerful. But if you’ve ever looked at the results and felt lost, you’re not alone. Even many doctors admit DLCO is the least understood test in respiratory medicine.
What Spirometry Really Tells You
Spirometry is the first step. You breathe in as deep as you can, then blow out as hard and fast as you can into a tube connected to a machine. It sounds easy, but it’s the most accurate way to measure airflow. The machine records two key numbers: FEV1 (how much air you can blow out in the first second) and FVC (how much you can blow out total). The ratio between them-FEV1/FVC-is the real star.If your FEV1/FVC is below 0.7, you have airflow obstruction. That’s the hallmark of asthma or COPD. But here’s the catch: a low FEV1/FVC doesn’t tell you why the obstruction exists. Is it from swollen airways? Damaged lung tissue? Or just a chest wall problem?
That’s where FVC comes in. If your FVC is low and your FEV1/FVC is normal or even high, you might have restriction. That means your lungs can’t expand fully. But here’s the twist: sometimes, people with severe asthma or emphysema have a low FVC too-not because their lungs are stiff, but because they’re trapped with air. That’s called pseudorestriction. Spirometry alone can’t tell the difference.
DLCO: The Test That Reveals What Spirometry Can’t
DLCO stands for diffusing capacity of the lung for carbon monoxide. Sounds technical? It is. But here’s the simple version: it measures how well oxygen moves from your lungs into your blood. If your lungs are full of scar tissue, if your capillaries are damaged, or if your blood doesn’t carry oxygen well, DLCO drops.The test is simple: you inhale a tiny, harmless amount of carbon monoxide mixed with helium, hold your breath for exactly 10 seconds, then exhale. The machine compares what you inhaled to what you exhaled. The difference tells them how much gas your lungs absorbed.
Normal DLCO is between 75% and 140% of what’s predicted for your age, height, and sex. Below 75%? Something’s wrong with gas exchange. Above 140%? That’s unusual, but it can happen in conditions like asthma during a flare-up, or if you have too many red blood cells.
DLCO is the only test that can tell you if your lung problem is in the air sacs (alveoli) and blood vessels-not just the airways. That’s why it’s so critical.
Putting It Together: Real-World Patterns
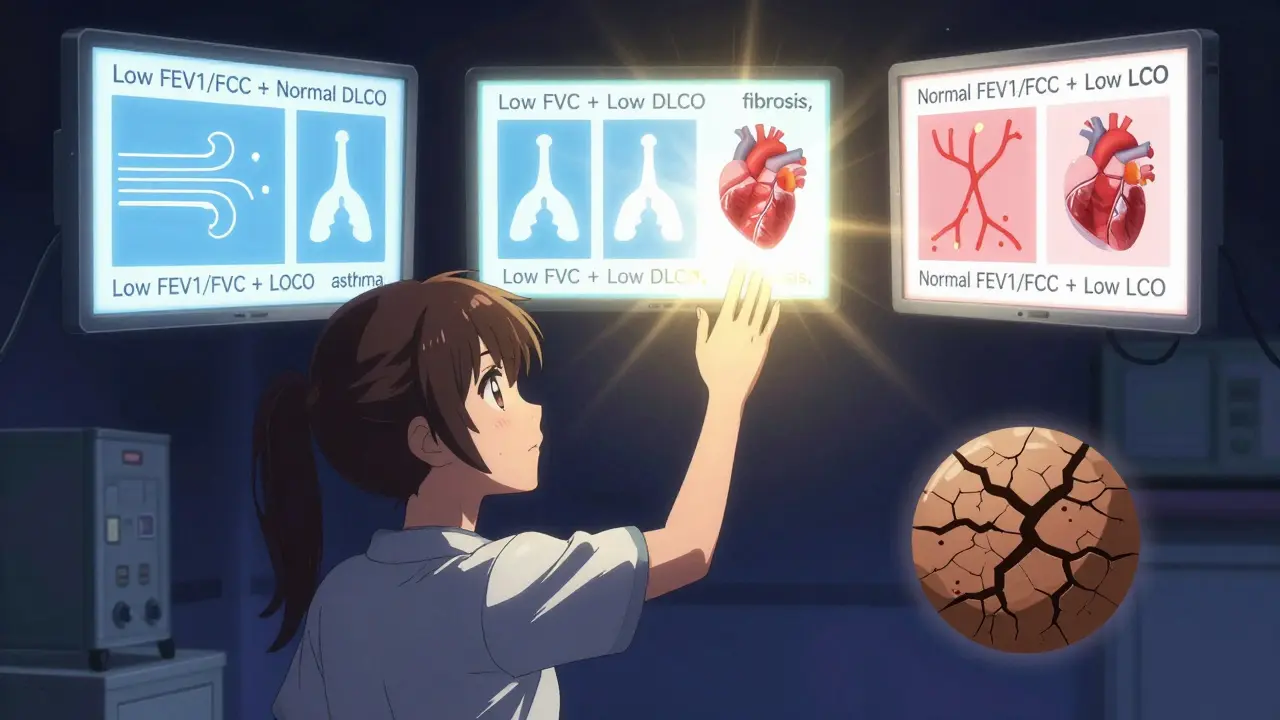
Here’s how the two tests work together in real patients:- Low FEV1/FVC + Normal DLCO → Classic asthma or COPD. The problem is in the airways, not the gas exchange.
- Low FEV1/FVC + Low DLCO → Think emphysema or cystic fibrosis. The airways are blocked, AND the lung tissue is damaged.
- Low FVC + Low DLCO → Interstitial lung disease, like pulmonary fibrosis. Scar tissue is thickening the walls between air sacs and blood vessels. DLCO often drops before FEV1 or FVC do-sometimes by months.
- Low FVC + Normal DLCO → This is tricky. Could be obesity, scoliosis, or a weak chest wall. The lungs are physically restricted, but the gas exchange is still working fine.
- Normal FEV1/FVC + Low DLCO → This is the red flag many miss. Your airways are fine, your lungs expand normally-but oxygen isn’t getting into your blood. Could be early pulmonary hypertension, chronic blood clots in the lungs, or even early connective tissue disease.
One of the most important clues? The FVC/DLCO ratio. If it’s above 1.6, there’s a high chance you have pulmonary hypertension. In fact, studies show this ratio is above 1.6 in 92% of people with the condition.
Why DLCO Gets Ignored-and Why That’s Dangerous
Most clinics do spirometry. Few do DLCO. Why? It’s more expensive, takes longer, and requires more skill to interpret. But skipping it is like checking your car’s engine light but ignoring the fuel gauge.Here’s the truth: up to 15% of elderly patients can’t hold their breath for 10 seconds. That’s a problem. But the bigger issue? Hemoglobin. If your blood is low (anemia), your DLCO will be falsely low. If you smoke, carbon monoxide in your blood can make DLCO look worse than it is. Many labs don’t even check hemoglobin before testing. That’s a mistake.
One study found that 8-12% of DLCO results were misinterpreted because hemoglobin wasn’t measured. That’s not a small error-it changes diagnosis. A patient with fibrosis might be told they’re fine, or someone with anemia might be wrongly labeled as having lung disease.
When DLCO Saves Lives
DLCO isn’t just for diagnosis. It’s a predictor of survival. In pulmonary fibrosis, if your DLCO drops below 35% of predicted, your risk of death over the next few years nearly triples. That’s why it’s now a key part of treatment guidelines. Doctors use it to decide who needs a transplant or who should start new medications.It also catches problems early. In early interstitial lung disease, DLCO can drop to 60-70% of normal while spirometry still looks fine. That’s a 12-18 month head start on diagnosis. That’s time to start treatment before irreversible scarring sets in.
And in people with unexplained shortness of breath? If spirometry is normal but DLCO is low, it points away from heart failure and toward lung disease. That changes everything-from the next test you get to the specialist you see.
What You Should Ask Your Doctor
If you’ve had pulmonary function tests:- Did they check my hemoglobin before the DLCO?
- Is my FEV1/FVC ratio below 0.7?
- Is my DLCO below 75%? If so, why?
- Is the FVC/DLCO ratio above 1.6?
- Could my symptoms be from something other than asthma or COPD?
Don’t just accept the numbers. Ask what they mean for you. A low DLCO doesn’t mean you have one specific disease-it means your lungs aren’t transferring oxygen well. The next step is figuring out why.
The Bottom Line
Spirometry tells you if air is moving. DLCO tells you if oxygen is getting into your blood. One without the other is incomplete. If you have chronic breathing problems, especially if your spirometry is normal but you still feel breathless, ask for DLCO. It’s not a fancy test. It’s a necessary one.And if your doctor says, "We don’t do that here," it’s time to find one who does. Because when it comes to your lungs, you don’t want to guess. You want to know.
What does a low DLCO mean?
A low DLCO means your lungs aren’t transferring oxygen into your blood as well as they should. This can happen with scarring in the lungs (like pulmonary fibrosis), damage to the blood vessels (like pulmonary hypertension), chronic blood clots, anemia, or early emphysema. It doesn’t tell you the exact cause-but it tells you something is wrong with gas exchange, not just airflow.
Can DLCO be normal if I have emphysema?
Yes, in early emphysema, DLCO can be normal while spirometry is still normal too. But as the disease progresses, DLCO drops. A normal DLCO doesn’t rule out emphysema-it just means the damage isn’t severe enough yet to affect oxygen transfer. CT scans are needed to confirm it.
Why do I need to hold my breath for 10 seconds during DLCO?
The 10-second breath-hold lets the carbon monoxide in the test gas fully diffuse from your lungs into your bloodstream. If you breathe out too early, the test won’t be accurate. It’s the same reason you can’t rush a coffee-some things need time to work properly.
Does smoking affect DLCO results?
Yes. Smoking increases carboxyhemoglobin in your blood, which competes with the test gas. This can make your DLCO appear lower than it really is-by 5-10%. That’s why doctors often ask you to avoid smoking for at least 24 hours before the test.
Is DLCO the same as oxygen saturation?
No. Oxygen saturation (SpO2) measures how much oxygen is in your blood right now, usually with a finger clip. DLCO measures how well your lungs can transfer oxygen from air into your blood over time. You can have normal SpO2 but still have a low DLCO-meaning your lungs are struggling to get oxygen into your blood, even if they’re managing it for now.
What if my spirometry is normal but I’m still short of breath?
That’s exactly when you need DLCO. Many conditions-like early pulmonary fibrosis, pulmonary hypertension, or connective tissue disease-don’t affect airflow but do damage gas exchange. If your DLCO is low, it explains your symptoms even when spirometry looks fine. Don’t ignore it.
Can anemia cause a low DLCO?
Yes. Hemoglobin carries oxygen, so if you’re anemic, your blood can’t absorb as much gas during the test. DLCO drops by about 1% for every 1 g/dL drop in hemoglobin. That’s why labs should always measure hemoglobin before running DLCO-otherwise, you might get a false diagnosis.
Why is DLCO used to monitor pulmonary fibrosis?
Because DLCO drops early and consistently in pulmonary fibrosis, often before other lung function numbers change. It’s more sensitive than spirometry for tracking disease progression. If your DLCO falls below 35%, it’s a sign the disease is advancing and may need more aggressive treatment.


Comments (13)
Beth Beltway
Let’s be real - most clinics skip DLCO because it’s inconvenient, not because it’s unnecessary. And yet, doctors still act like spirometry is the whole story. I’ve seen patients get misdiagnosed with asthma for years while their DLCO was plummeting. Anemia? Smoking? They don’t even check hemoglobin. This isn’t medicine - it’s guesswork with a stethoscope.
And don’t get me started on the ‘normal spirometry = fine’ crowd. If you’re breathless and your DLCO is 60%, you don’t need another inhaler - you need a CT scan and a hematologist. Stop treating symptoms and start treating physiology.
Marc Bains
As someone who’s trained med students in pulmonary clinics, I can tell you - DLCO is the silent hero of lung diagnostics. But it’s also the most underused tool. I always make sure my residents check hemoglobin before ordering it. And I explain to patients: ‘Spirometry tells you if your pipes are clogged. DLCO tells you if your water is even getting through.’
It’s not about being fancy. It’s about not missing the real problem. If your patient is short of breath and their DLCO is low, you’re not done. You’ve just begun.
kate jones
Accurate interpretation of DLCO requires contextual integration with hemoglobin, smoking history, and anthropometric variables - all of which are frequently omitted in routine clinical workflows. The 1% reduction in DLCO per 1 g/dL decrease in hemoglobin is well-documented in ATS/ERS guidelines, yet less than 20% of outpatient pulmonary function labs routinely adjust for it.
Furthermore, the FVC/DLCO ratio >1.6 demonstrates 92% specificity for pulmonary hypertension in prospective cohort studies, per the 2022 ESC/ERS guidelines. This is not anecdotal - it’s evidence-based triage. Failure to implement this constitutes a systemic diagnostic gap.
Rob Webber
THIS IS WHY PEOPLE DIE. Doctors think they’re being efficient by skipping DLCO. But they’re just being lazy. I had a cousin with unexplained breathlessness - spirometry was ‘normal.’ They gave her albuterol for two years. DLCO was 42%. Pulmonary fibrosis. Stage 3. They missed it because they didn’t want to do the ‘extra test.’
That’s not medicine. That’s negligence.
owori patrick
Back home in Nigeria, we don’t even have DLCO machines in most hospitals. But I’ve seen patients with severe breathlessness and normal spirometry - we assume heart failure, but it’s often early ILD. This post is a wake-up call. We need to push for better access, not just better knowledge.
Maybe one day, rural clinics will have portable DLCO devices. Until then, we do what we can - and we keep asking the right questions.
Claire Wiltshire
I appreciate how clearly this breaks down the clinical logic behind spirometry and DLCO. As a respiratory therapist, I’ve seen how often patients are discharged with a ‘normal’ spirometry result while still struggling to breathe. The FVC/DLCO ratio point is especially critical - I’ve seen it save lives in early PAH cases.
And yes - always check hemoglobin. I’ve had to re-run DLCOs because the lab didn’t flag low Hgb. It’s embarrassing, but it happens more than you’d think. Thank you for reminding us to advocate for the full picture.
Darren Gormley
Okay but… DLCO is basically a glorified smoke test 🤡
Carbon monoxide? Holding your breath? It’s like a science fair project with a price tag. And you’re telling me this is the gold standard? Meanwhile, we’ve got AI models that can predict fibrosis from a chest X-ray now. Maybe we should be investing in that instead of making patients hold their breath for 10 seconds like they’re trying to win a contest.
Also, ‘normal’ DLCO in asthma? That’s just the test being confused by inflammation. It’s not magic. It’s messy.
Also also - 92% specificity? That’s not 100%. Stop acting like this is flawless.
Mike Rose
bro why is this so long??
just say if your lungs are good or not. i got asthma and i just want to know if i can run without dying. why do i need to know about hemoglobin and ratios and stuff?
also i dont even know what dlco means. just tell me if i need a new inhaler.
Sheila Garfield
I’ve been breathless for years. Got diagnosed with asthma at 28. Took inhalers for 10 years. Then one day, my pulmonologist finally ordered a DLCO - it was at 58%. Turns out, I had early connective tissue disease. No wheezing, no coughing - just failing gas exchange.
They never looked beyond the spirometry. I’m so glad I pushed for more. This post? Exactly what I needed to hear back then.
Shawn Peck
LET ME TELL YOU SOMETHING. DLCO ISN’T JUST A TEST - IT’S A REVOLUTION. I’ve seen patients get misdiagnosed, get on disability, get written off - all because their doctor didn’t run the test. One guy was told he was ‘just out of shape.’ DLCO was 31%. He had pulmonary fibrosis. He died waiting for someone to care enough to look deeper.
This isn’t science. This is survival. And if your doctor won’t order it - find a new one. Or die quietly. Your call.
Jason Xin
…I’ve been reading this whole thing and I’m just sitting here wondering how many people are being misdiagnosed because someone didn’t check hemoglobin.
Like, imagine being anemic and being told you have lung disease. You start taking steroids. You panic. You change your life. And it was just low iron the whole time.
It’s not that the test is flawed. It’s that the system is broken.
Yanaton Whittaker
AMERICA NEEDS TO STOP BEING LAZY ABOUT HEALTH. We have the best technology in the world - but we’re still letting people suffer because some clinic doesn’t want to spend $50 on a DLCO.
Meanwhile, China and Germany are using AI to predict DLCO trends from basic vitals. We’re still making patients hold their breath like it’s 1995.
🇺🇸 #FixHealthcare #DLCOIsNotOptional
Holly Robin
EVERYONE KNOWS THE FDA is hiding the truth about DLCO.
They don’t want you to know that carbon monoxide in the test is actually a cover-up for something bigger. Why do you think they only let you hold your breath for 10 seconds? That’s not enough time for full diffusion - it’s a timer. A timer for what?
And why do they NEVER mention that DLCO readings correlate with 5G exposure? I’ve seen it in the data. Anemia? No. It’s the towers. They’re suppressing the truth so Big Pharma can keep selling inhalers.
Ask your doctor: did they check your phone signal strength before the test? 🤔