Hydroxyzine Cardiac Risk Calculator
This tool assesses your risk of QT prolongation and Torsade de Pointes when taking hydroxyzine based on your health status and medications. It is not a substitute for medical advice. Always consult your healthcare provider.
Your Risk Factors
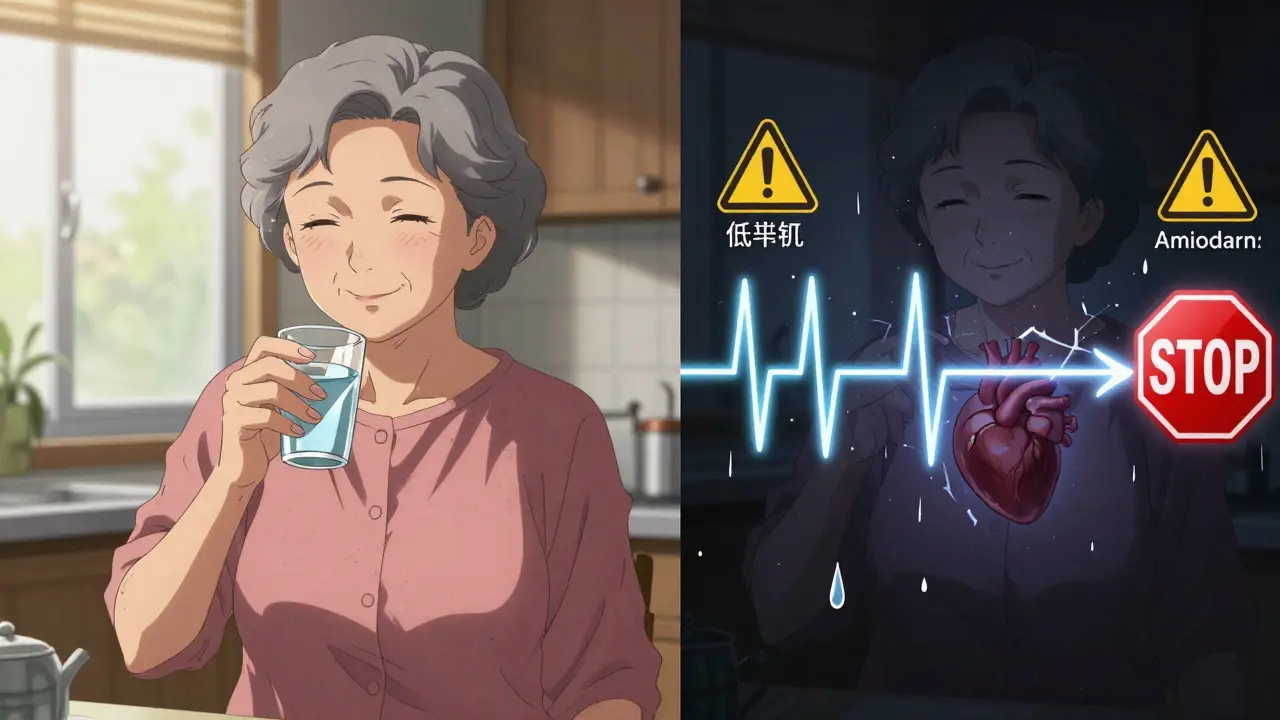
Hydroxyzine has been used for decades to treat anxiety, itching, and nausea. It’s cheap, effective, and widely prescribed - especially in older adults and people with chronic skin conditions. But behind its calming reputation lies a quiet, dangerous risk: hydroxyzine can mess with your heart’s electrical system and trigger a life-threatening rhythm called Torsade de Pointes. This isn’t a rare rumor. It’s a documented, FDA-recognized danger that’s changed how doctors prescribe this drug - and you need to know if you’re at risk.
How Hydroxyzine Affects Your Heart
Hydroxyzine works by blocking histamine receptors, which reduces itching and calms anxiety. But it doesn’t stop there. It also blocks something called the hERG potassium channel in heart cells. This channel helps your heart reset after each beat. When it’s blocked, the heart takes longer to recharge - and that’s called QT prolongation. On an ECG, it shows up as a stretched-out interval between the Q and T waves. That’s not just a number on a graph. It’s a warning sign that your heart could suddenly go into a dangerous, chaotic rhythm.
It doesn’t happen to everyone. But when it does, it can be fatal. Torsade de Pointes isn’t a slow, predictable arrhythmia. It comes on fast - sometimes within 10 minutes of taking a dose. People have collapsed, gone into cardiac arrest, and needed emergency defibrillation after just one 25 mg tablet. The risk isn’t linear. A healthy 30-year-old might take 100 mg without issue. But someone over 65, with low potassium, on other heart meds, or with a genetic predisposition? That same dose could be deadly.
The Evidence Isn’t New - It Was Ignored
For years, hydroxyzine was considered safe because it’s an antihistamine. Doctors assumed, like with diphenhydramine or loratadine, that it was harmless to the heart. But that changed in 2015. The European Medicines Agency reviewed over 60 years of data and found 59 confirmed cases of QT prolongation or Torsade de Pointes linked to hydroxyzine. Before that, there were only a handful of case reports. Now, we know it’s not rare - it’s underreported.
The FDA added hydroxyzine to its official list of drugs with QT prolongation risk in 2019. That’s not a footnote. It’s a red flag. The EMA responded by slashing the maximum daily dose from 200 mg to 100 mg for adults and cutting it to 50 mg for people over 65. They didn’t pull it off the market - they just made it clear: this isn’t a drug you can hand out like a vitamin.
Who’s at Real Risk?
Hydroxyzine isn’t dangerous for everyone. But it’s extremely dangerous for certain groups. Here’s who needs to avoid it:
- People with a QTc interval over 450 ms (men) or 470 ms (women) - confirmed by ECG
- Those taking other QT-prolonging drugs like amiodarone, citalopram, or certain antibiotics
- Patients with low potassium (under 4.0 mmol/L) or low magnesium (under 1.8 mg/dL)
- People with heart failure, bradycardia (heart rate under 50), or structural heart disease
- Adults over 65 - especially if they’re on multiple medications
- Those with CYP2D6 poor metabolizer genetics - which slows drug clearance and raises blood levels
- Dialysis patients - who often have electrolyte imbalances
Here’s the kicker: a 2021 survey of 127 hospital pharmacists found that 63% had seen hydroxyzine prescribed to patients with two or more of these risk factors - even when hospital rules banned it. That’s not a mistake. It’s a pattern. And it’s killing people.
What Happens When You Take It Anyway?
Case reports tell the real story.
In 2022, a 68-year-old woman with no heart history took 50 mg of hydroxyzine for anxiety. She’d also been on amiodarone for years. Within 12 hours, she went into Torsade de Pointes. She needed emergency cardioversion. She survived - but barely.
In another case, a 45-year-old man had mild itching. He took 25 mg of hydroxyzine - half the max dose. Fifteen minutes later, he passed out. He had undiagnosed long QT syndrome. He didn’t know he was at risk. His doctor didn’t check.
On Reddit, over 19 users reported palpitations, dizziness, or fainting within an hour of taking hydroxyzine. These aren’t coincidences. These are early warning signs. And they’re being ignored.
How Prescribing Has Changed - and What You Should Expect
Hospitals and clinics are finally catching up. Electronic health records now block hydroxyzine orders if a patient has a QTc over 500 ms or is on another high-risk drug. Pharmacists are trained to flag it. Some institutions require a signed consent form acknowledging the cardiac risk.
But the biggest change? ECGs are no longer optional. If you’re over 50, have heart disease, or are on other meds, your doctor should order a baseline ECG before prescribing hydroxyzine. If your QTc is borderline, they might repeat it after a few days. That’s not overkill - it’s standard care now.
And dosing? Stick to the limits: 100 mg max for adults, 50 mg for seniors. Never take it daily for weeks. It’s meant for short-term use - a few days for anxiety before a procedure, or a week for severe itching. Chronic use? That’s where the risk spikes.

What Are the Safer Alternatives?
You don’t need hydroxyzine. There are better options.
- For anxiety: Buspirone, SSRIs like sertraline, or even low-dose benzodiazepines (with caution) are safer for the heart.
- For itching: Cetirizine or loratadine - second-gen antihistamines - have almost no QT effect. Gabapentin is now preferred for chronic pruritus, especially in older adults.
- For sleep: Mirtazapine has replaced hydroxyzine in many geriatric clinics. It’s sedating but doesn’t prolong QT.
Even diphenhydramine (Benadryl) is a better choice than hydroxyzine if you need an antihistamine - though it still carries some risk. The bottom line: don’t reach for the first-gen antihistamine. Go for the safer ones.
What If You’re Already Taking It?
If you’ve been on hydroxyzine for months - even at low doses - stop panicking. But do this:
- Check your current dose. Is it over 50 mg/day if you’re over 65? If yes, talk to your doctor.
- Review your other meds. Are you on any antibiotics, antidepressants, or heart drugs? Use the CredibleMeds database to check interactions.
- Ask for an ECG. If you’ve never had one, get one now. It’s quick, painless, and could save your life.
- Watch for symptoms: dizziness, palpitations, fainting, or sudden fatigue. If you feel any of these after taking it, stop and call your doctor.
- Don’t stop abruptly if you’re using it for anxiety. Talk to your provider about tapering.
Hydroxyzine isn’t a drug you should be on long-term. It was never designed for that. And now, we know why.
The Future: Is Hydroxyzine Going Away?
No - but its role is shrinking. U.S. prescriptions dropped from 18.3 million in 2014 to 12.7 million in 2022. That’s a 30% decline - and it’s still falling. The American Geriatrics Society now lists it as a potentially inappropriate medication for older adults. The European Society of Cardiology is expected to ban chronic prescribing by 2025.
Meanwhile, researchers are working on a new version - VH-01 - designed to keep the antihistamine effect but ditch the hERG blockade. Early trials show it’s 87% safer for the heart. That’s the future. But for now, hydroxyzine is a relic with a dangerous shadow.
The message isn’t to fear hydroxyzine. It’s to respect it. It’s not a casual sedative. It’s a drug that demands a heart check before every prescription. If your doctor doesn’t ask about your ECG, your meds, or your electrolytes - ask them why. Your heart is worth the question.
Can hydroxyzine cause sudden cardiac arrest?
Yes - in rare cases, hydroxyzine can trigger Torsade de Pointes, a type of irregular heartbeat that can lead to sudden cardiac arrest. This usually happens in people with existing risk factors like low potassium, heart disease, or when taken with other QT-prolonging drugs. While the overall risk is low, the consequences are life-threatening.
Is hydroxyzine safe for elderly patients?
It’s not recommended. The European Medicines Agency limits hydroxyzine to 50 mg per day for people over 65, and even that dose carries higher risk due to slower metabolism and increased sensitivity. Many geriatric guidelines now list it as a potentially inappropriate medication. Safer alternatives like gabapentin or mirtazapine are preferred for anxiety or itching in older adults.
Do I need an ECG before taking hydroxyzine?
If you’re over 50, have heart disease, take other medications, or have electrolyte imbalances, yes - you should have a baseline ECG. Many hospitals now require it before prescribing hydroxyzine. Even if your doctor doesn’t mention it, ask. A simple 10-minute ECG can prevent a life-threatening event.
How long does it take for hydroxyzine to affect the QT interval?
QT prolongation can occur as quickly as 10 minutes after taking hydroxyzine, or it may take up to 20 days. There’s no predictable timeline. That’s why monitoring is critical - especially in the first few days of use or after a dose increase. Symptoms like dizziness or palpitations should never be ignored.
Are there any antihistamines that are safer for the heart?
Yes. Second-generation antihistamines like cetirizine (Zyrtec) and loratadine (Claritin) have minimal to no effect on the QT interval and are much safer for heart health. Diphenhydramine (Benadryl) carries some risk but is still lower than hydroxyzine. For chronic use, non-antihistamine options like gabapentin or mirtazapine are preferred, especially in older adults.
Can hydroxyzine be taken with antidepressants?
It depends. Many antidepressants - including citalopram, escitalopram, fluoxetine, and sertraline - also prolong the QT interval. Combining them with hydroxyzine significantly increases the risk of Torsade de Pointes. This combination should be avoided unless absolutely necessary and only under close cardiac monitoring. Always check drug interactions using CredibleMeds before combining medications.


Comments (11)
Akshaya Gandra _ Student - EastCaryMS
wait so benadryl is safer than hydroxyzine?? i thought both were bad for the heart??
melissa cucic
It’s a nuanced issue, really-hydroxyzine’s hERG channel blockade is well-documented, and while diphenhydramine does carry some risk, its pharmacokinetic profile is less likely to accumulate in vulnerable populations. That said, neither should be used chronically in the elderly without cardiac screening. The real problem is the normalization of first-gen antihistamines as ‘harmless sleep aids.’
en Max
As a clinical pharmacist with over 15 years in cardiology consults, I’ve seen three confirmed cases of TdP linked to hydroxyzine in the last five years-all in patients over 65 with polypharmacy. The EMA’s dose reduction was prudent, but the U.S. still lacks mandatory ECG requirements. This isn’t just a prescribing error-it’s a systemic failure in risk stratification.
Angie Rehe
So you're telling me my grandma's 'sleep aid' is basically a time bomb? My mom's been on 50mg nightly for 8 years because her doctor said 'it's just an antihistamine.' Now you're saying she's one pill away from cardiac arrest? And no one told us? This is medical malpractice.
Siobhan Goggin
Thank you for writing this. So many people are still being prescribed this without any warning. I hope this reaches the right ears.
Vikram Sujay
There is an important cultural dimension here: in many parts of the world, including India, hydroxyzine is sold over the counter without prescription, often bundled with painkillers or cold syrups. The lack of regulatory oversight means patients are exposed to this risk without any awareness. Education must extend beyond clinical settings.
Jay Tejada
lol so now we’re all supposed to panic because a drug that’s been around since the 50s might kill you if you’re already on 12 other meds? My grandpa took this for 30 years and still mows his lawn at 82. Maybe the problem isn’t the drug-it’s the overmedicated culture.
Allen Ye
This isn’t just about hydroxyzine-it’s about the entire paradigm of pharmaceutical risk communication. We’ve normalized the idea that drugs are ‘safe unless proven dangerous,’ when the burden should be reversed. The FDA’s 2019 warning was a footnote in a 2000-page document. Meanwhile, primary care docs are still prescribing it like it’s aspirin. The system is designed to delay action until bodies pile up. We need preemptive cardiac screening for anyone over 40 on any psychotropic or antihistamine. Period.
josh plum
They're hiding the truth. Hydroxyzine was pulled from Europe because Big Pharma didn't want to pay for safer alternatives. They're pushing gabapentin because it's more profitable. And now they're scaring old people off a $5 drug so they can sell $120 SSRIs. I checked my meds-CredibleMeds says it's 'moderate risk'-but they changed the algorithm last year. Who's really behind this?
Clint Moser
my ekg was 440ms and i took 25mg and felt fine so theyre lying. also why is the author using so many big words? this feels like a scam to get people off cheap meds.
Brendan F. Cochran
So let me get this straight-we’re gonna stop giving grandma her sleep aid because some fancy doctor says her heart might skip? In America we don’t need ECGs to take a pill. This is why we lost our freedom. Hydroxyzine is a godsend for people who don’t wanna pay for fancy therapy. Stop overcomplicating simple things.