Getting the right amount of liquid medicine isn’t just about following the label-it’s about avoiding real harm. Every year, thousands of children and adults receive incorrect doses of liquid medications because the tool used to measure it was wrong, unclear, or mismatched with the prescription. This isn’t rare. Studies show that 15-43% of caregivers make dangerous mistakes when measuring liquid drugs at home, and up to 20% of all liquid medication errors come from using the wrong dosing device. The problem isn’t that people are careless. It’s that the system is designed to fail.
Why Household Spoons and Cups Are Dangerous
A teaspoon isn’t a teaspoon. A tablespoon isn’t a tablespoon. When caregivers use kitchen spoons to measure liquid medicine, they’re guessing. A regular teaspoon holds anywhere from 2.5 mL to 7 mL-far outside the safe range for a child’s dose. The Institute for Safe Medication Practices found that household spoons are responsible for 40% of pediatric dosing errors. That’s not a typo. It’s a public health issue. Dosing cups are slightly better, but still flawed. Most come with too many markings-lines for 1 mL, 2 mL, 5 mL, 10 mL, 15 mL, even 30 mL-on a single cup meant for a 5 mL dose. That visual clutter confuses people. A 2013 JAMA Network study found that 81.1% of dosing cups included unnecessary lines, and caregivers using them made errors 43% of the time when measuring a 2.5 mL dose. Why? Parallax error. If you’re looking at the cup from above or below eye level, the liquid’s curve (called the meniscus) looks wrong. Most people don’t know how to read it properly.The Only Device That Consistently Works: Oral Syringes
Oral syringes are the gold standard. They don’t rely on your angle. They don’t have extra lines. They show exact volumes in 0.1 mL increments. For doses under 5 mL-common in pediatric and geriatric care-they’re the only reliable choice. A 2009 study in the Annals of Pharmacotherapy showed that when measuring a 5 mL dose, 66.7% of people using an oral syringe got it right within ±0.5 mL. Only 14.6% did with a dosing cup. Even better: for a 2.5 mL dose, syringe error rates were just 4%. Cups? 43%. Droppers? 22%. Spoons? Up to 15% off target. The problem isn’t accuracy-it’s perception. People think syringes are hard to use. In reality, they’re easier once you learn how. A 2022 survey found that while 87% of caregivers said cups were easy to use, only 63% felt the same about syringes. But after trying them, 76% of Amazon reviewers praised syringes for precision and spill-free dosing. One parent wrote: “The 1 mL syringe with 0.1 mL markings saved my infant from an overdose when the dose was 1.6 mL. The cup only had 1 mL and 2 mL lines.”What the Experts Say: Milliliters Only
The American Academy of Pediatrics, the FDA, the United States Pharmacopeia (USP), and the National Council for Prescription Drug Programs all agree: use milliliters (mL) only. No teaspoons. No tablespoons. No “cc” or “tsp.” The FDA’s 2022 guidance made this crystal clear: “The use of teaspoons and tablespoons on labels may encourage the use of non-calibrated household spoons.” That’s why, since 2015, 34 U.S. states have passed laws requiring metric-only labeling on liquid medications. Yet, a 2023 FDA audit still found that 28% of liquid prescriptions include teaspoon or tablespoon instructions. The USP sets the accuracy bar: any device must measure within 10% of the prescribed dose. Oral syringes consistently meet this. Dosing cups? Often don’t. Spoons? Almost never.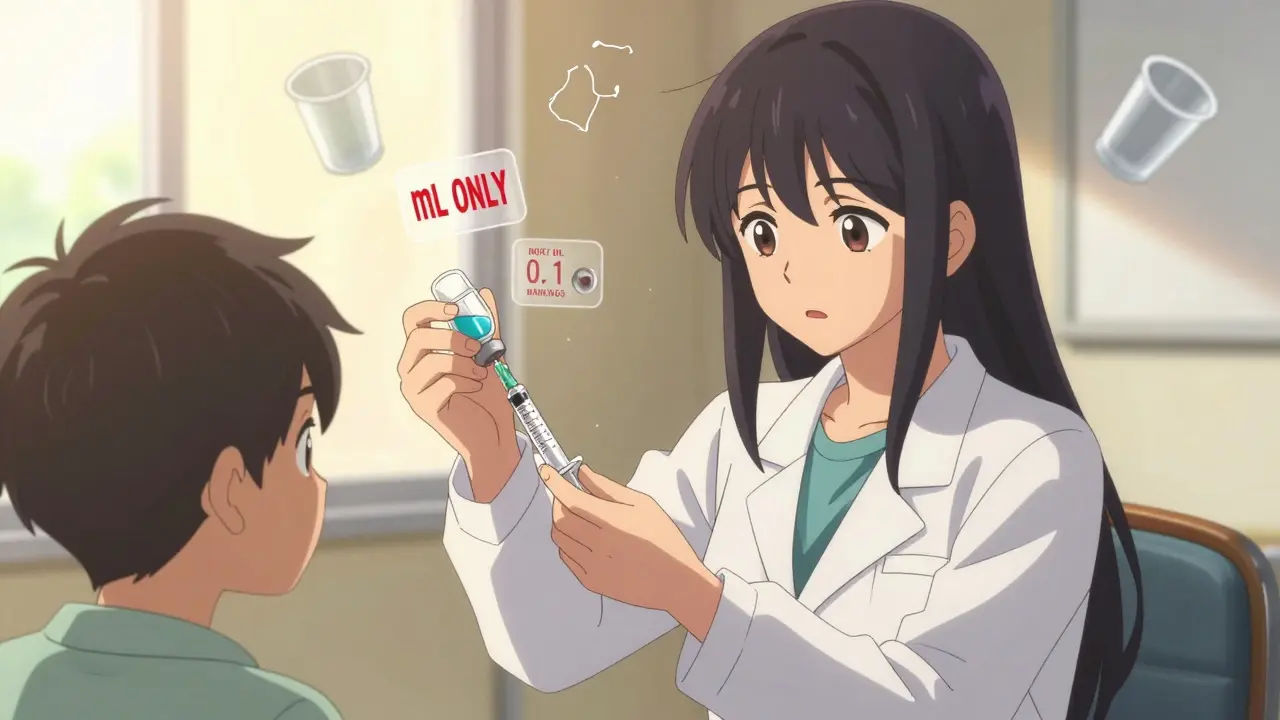
How to Choose the Right Dosing Device
Not all syringes are created equal. Here’s what to look for:- For doses under 5 mL: Use a 1 mL or 5 mL syringe with 0.1 mL markings.
- For doses between 5-10 mL: Use a 10 mL syringe with 0.1 or 0.2 mL markings.
- For doses over 10 mL: A dosing cup with only two or three clear markings (e.g., 10 mL, 15 mL) may be acceptable-but only if it’s labeled in mL and matches the prescription exactly.
- Avoid: Anything labeled in teaspoons, tablespoons, or fluid ounces. Anything with more than 4 markings. Anything that doesn’t come with the medication.
How to Use an Oral Syringe Correctly
Even the best device fails if used wrong. Teach this simple 3-step method:- Draw the liquid: Insert the tip below the surface of the medicine. Pull the plunger slowly until the top edge of the plunger aligns with the correct mark. Don’t rush.
- Remove air bubbles: Gently tap the syringe to make bubbles rise. Push the plunger slightly to push them out, then re-draw to the right mark.
- Read at eye level: Hold the syringe straight. Look at the plunger from the side, not from above or below. The top edge of the plunger should line up with the number on the barrel.

What Pharmacies and Providers Must Do
It’s not just up to the caregiver. Pharmacies and clinics have a duty to prevent errors.- Include a syringe with every liquid prescription under 10 mL. Don’t wait for the patient to ask.
- Match the label to the device. If the label says “5 mL,” the syringe must say “5 mL.” No exceptions.
- Use the teach-back method. Ask the caregiver: “Can you show me how you’ll give this dose?” If they can’t, don’t send them home.
- Attach QR codes. Kaiser Permanente started putting QR codes on labels that link to 60-second video demos. Usage increased syringe adoption by 41%.
The Bigger Picture: Progress and Gaps
There’s been real progress. Between 2015 and 2022, pediatric liquid medication errors dropped 37% in U.S. emergency rooms. That’s thanks to standardized labeling, syringe distribution, and education. But big gaps remain:- Only 35% of pediatric liquid prescriptions include an oral syringe.
- 63% of low-income patients get lower-quality devices than wealthier patients.
- 24.3% of OTC pediatric meds still don’t include any dosing device.
- Only 12 states regularly check pharmacy compliance with dosing rules.
What You Can Do Today
If you’re giving liquid medicine:- Ask for an oral syringe. Don’t accept a cup or spoon.
- Check that the label says “mL”-not “tsp” or “tbsp.”
- Use the syringe at eye level. No guessing.
- Practice with water before giving the real dose.
- If you’re unsure, call the pharmacy. Ask: “Is this dose safe? Can you show me how to measure it?”
- Prescribe in mL only.
- Include a syringe with every liquid script under 10 mL.
- Use the teach-back method. Every time.
- Update your labels to match NCPDP standards.
Why can't I just use a kitchen spoon to give liquid medicine?
Kitchen spoons aren’t calibrated. A teaspoon can hold anywhere from 2.5 mL to 7 mL, depending on how you fill it. A child’s dose of 5 mL could easily become 7 mL-or 3 mL-leading to overdose or underdose. The Institute for Safe Medication Practices says household spoons cause 40% of pediatric dosing errors. Always use a medical-grade device.
Are oral syringes really better than dosing cups?
Yes, especially for doses under 10 mL. Studies show oral syringes have error rates as low as 4% for small doses, while dosing cups have error rates up to 43%. Cups are prone to parallax error, confusing markings, and inaccurate meniscus reading. Syringes give exact volume control, even with 0.1 mL precision.
What should I look for on a dosing device label?
The device should only use milliliters (mL), not teaspoons or tablespoons. It should have minimal, clear markings that match the prescription exactly. Avoid devices with more than 4 lines. Look for leading zeros (e.g., 0.5 mL, not .5 mL) and no trailing zeros (e.g., 5 mL, not 5.0 mL). Always check that the unit on the device matches the label.
Why do some pharmacies still give out dosing cups?
Many pharmacies still use outdated practices or stock cheaper cups because they’re less expensive. Some assume caregivers prefer them, even though research shows syringes are safer. Only 35% of pediatric liquid prescriptions include a syringe, even though guidelines from the American Pharmacists Association and FDA have recommended them since 2011. It’s a system-wide failure, not a caregiver one.
Can I reuse an oral syringe for multiple doses?
No. Oral syringes should be used for one dose only and then discarded. Reusing them risks contamination, clogging, or inaccurate measurements due to residue buildup. Always use a new syringe for each dose, especially for children, elderly patients, or immunocompromised individuals.
What if the prescription says 5.0 mL? Should I use a syringe marked 5.0 mL?
No. Avoid syringes with markings like 5.0 mL. The FDA and USP recommend using 5 mL, not 5.0 mL, because trailing zeros can confuse people into thinking precision is needed beyond what the device can deliver. Use a syringe marked 5 mL. The decimal point in the prescription (5.0) doesn’t mean you need more precision-it’s just how the doctor typed it. The device should match the standard: 5 mL.
How can I check if I measured the dose correctly?
Use a digital kitchen scale. One milliliter of water weighs one gram. So a 5 mL dose should weigh 5 grams. If you measure the liquid in the syringe and it weighs 5.5 grams or 4.3 grams, you’ve made an error. This is the most reliable way to verify accuracy at home.


Comments (13)
Jennifer Phelps
Just used a syringe for my kid’s antibiotics last week and wow what a difference. No more guessing, no more spills. The 0.1 mL marks made it stupid simple. Why don’t pharmacies just give these out automatically?
Also, I didn’t know about the scale trick. Tested it with water-5 mL weighed exactly 5 grams. Mind blown.
jordan shiyangeni
It’s absolutely unacceptable that we still live in a society where parents are expected to be amateur pharmacists using kitchen utensils as medical instruments. The FDA has been screaming about this since 2015, yet 28% of prescriptions still use teaspoons? That’s not negligence-it’s institutional malpractice. The fact that 63% of low-income patients get inferior devices isn’t a coincidence; it’s systemic class-based healthcare violence. And don’t get me started on the fact that pharmacists still hand out dosing cups like they’re party favors. This isn’t a parenting issue-it’s a failure of the entire medical-industrial complex to prioritize safety over cost-cutting. We need mandatory federal audits, not suggestions. And if you’re still using a cup, you’re literally gambling with your child’s life.
Abner San Diego
Ugh. Another one of these ‘doctors know best’ rants. Look, I get it, syringes are fancy. But my grandma gave me medicine with a spoon and I turned out fine. We’re talking about a few mL here. You think every kid in the world has access to a $5 syringe? Meanwhile, people in Nigeria and India are using clean straws and droppers made from plastic bottles-because they have to. Stop acting like this is some first-world problem. The real issue is poverty, not punctuation on a label. And stop calling people careless. They’re just trying to keep their kids alive with what they’ve got.
Eileen Reilly
ok so i just tried using the syringe thing and i think i did it wrong? i thought you had to push the plunger to get the air out but then i saw a video and it said tap it? now im scared i overdosed my dog. also why do all these articles say 0.1 ml but my syringe says 0.10? is that different? and why is the cup free but the syringe costs $3? pharmacy is a scam.
steve ker
Oral syringes are for weak people. Real men use the teaspoon. You think your 0.1 mL precision matters when the medicine is 90% sugar water anyway? This is overengineering for people who can’t handle a little ambiguity. Also, why do Americans treat medicine like it’s rocket science? In Nigeria we just give the dose and move on. No apps. No scales. No QR codes. Life goes on.
Sonal Guha
Why are we still talking about mL? The metric system is a colonial relic. Why not use traditional Indian units like ‘dara’ or ‘tola’? They’re culturally grounded and more intuitive. Also, the whole syringe obsession is just Western medical imperialism. My aunt gave my cousin 2 ‘pinch’ doses of syrup with a spoon and he’s now a doctor. Precision is a myth. Trust the body.
TiM Vince
I’m from Japan. Here, every liquid medicine comes with a tiny plastic dropper-no syringe, no cup. It’s simple, cheap, and effective. We don’t have the same error rates because we don’t overcomplicate it. The key isn’t the tool-it’s the education. Teach people to read the scale once. No QR codes needed. And never, ever use a spoon. Even here, that’s considered dangerous.
Alice Elanora Shepherd
Thank you for this comprehensive, deeply necessary post. I’ve worked in pediatric nursing for 22 years, and I can tell you-this is the single most preventable cause of ER visits in children under five. The fact that 35% of prescriptions still don’t include a syringe is criminal. I always carry a few spare oral syringes in my bag and hand them out to parents who look confused. I’ve also started teaching the ‘eye-level, tap, check’ method during discharge. One mother cried because she’d been giving her son 7 mL when the prescription was 5 mL for months. She thought the ‘line’ was the bottom of the meniscus. No one ever told her. Please, if you’re reading this-ask for the syringe. Don’t wait for someone to offer it. And if you’re a provider-stop assuming they ‘know.’ They don’t. And that’s not their fault.
Christina Widodo
Wait, so if I use a syringe but my kid spits out half, do I re-dose? I’ve been doing that because I thought the dose was ‘lost.’ Also, can I wash and reuse the syringe if I rinse it with water? I don’t wanna waste money. And what if the bottle says 5 mL but the syringe says 5.0? Is that a trap? I feel like I’m being set up to fail.
Prachi Chauhan
Medicine is not math. It’s energy. The body knows what it needs. If you’re worried about 0.1 mL, you’re not healing-you’re controlling. In Ayurveda, we use ‘anjali’-a palmful. It’s intuitive. Precision is fear dressed as science. Let go. Trust the flow. The spoon is not the enemy. The mind that fears imperfection is.
Sona Chandra
THIS IS WHY MY SON ENDED UP IN THE HOSPITAL. I USED A KITCHEN SPOON BECAUSE THE PHARMACY WAS OUT OF SYRINGES AND NO ONE TOLD ME IT WAS DANGEROUS. NOW I’M TERRIFIED TO GIVE HIM ANY MEDICINE EVER AGAIN. WHO DO I SUE? THE PHARMACY? THE DOCTOR? THE GOVERNMENT? I JUST WANT MY BABY TO BE OKAY AND NO ONE CARES.
Rinky Tandon
Let’s be real: this isn’t about dosing. It’s about control. The medical establishment wants you dependent on their tools, their language, their precision. They profit from syringes, apps, QR codes, and fear. You think your 0.1 mL accuracy saves lives? Or does it just make you feel superior? My cousin in Kerala gives medicine with a finger dip. No device. No stress. No anxiety. And guess what? He’s never had a child hospitalized. Maybe the real error is believing that medicine must be measured to be holy.
Ben Kono
I’ve been using the same syringe for 3 months. Rinse it with hot water between doses. Works fine. Why pay $3 every time? Also, the scale trick is genius. I weighed my kid’s dose and it was 5.2g. So I pulled back a tiny bit. Now I’m confident. Also, why do they make syringes with 0.10 markings? It’s the same as 0.1. Stop overthinking it.