Tinea Versicolor Treatment Calculator
Your Situation
Treatment Recommendations
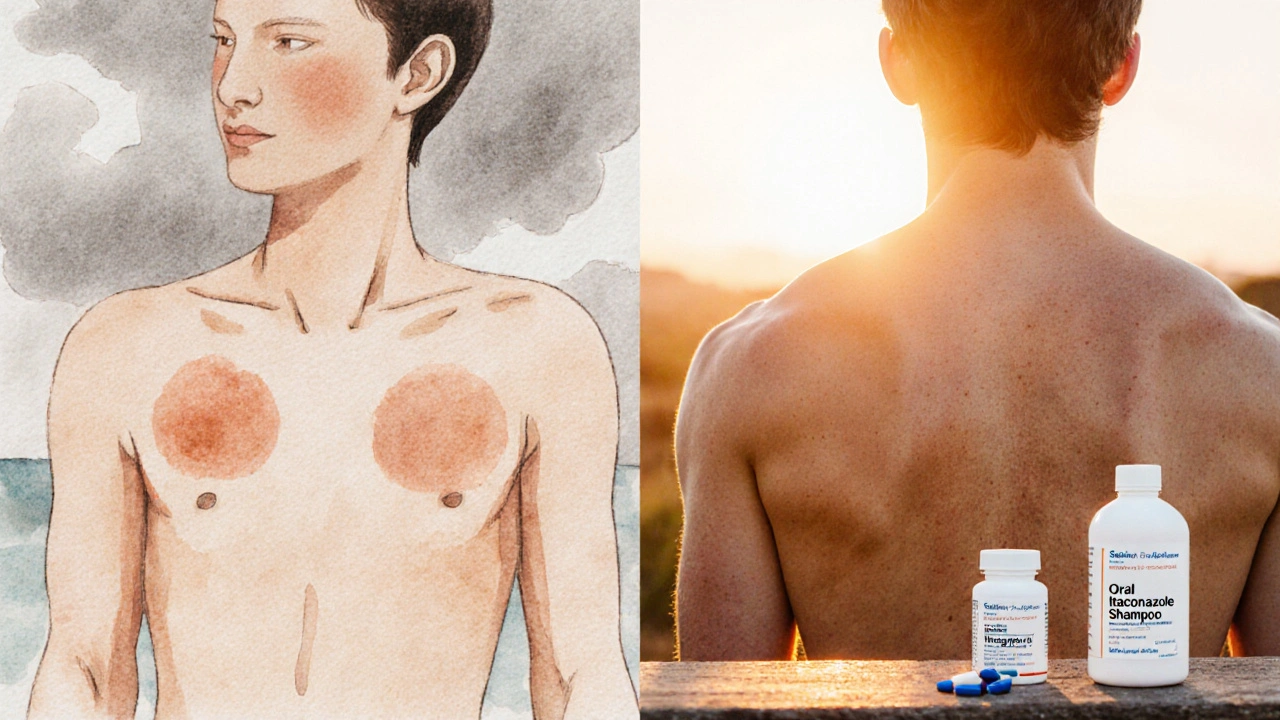
If you’ve ever noticed small, lighter or darker patches on your shoulders, chest, or back that seem to come and go, you might have dealt with tinea versicolor. While the condition is harmless, the visual impact can be frustrating, especially when the spots don’t fade with regular shampoo. This article breaks down how well antifungal medications work against the fungus, which treatments give the best results, and what you can do to keep the skin clear.
Key Takeaways
- Tinea versicolor is caused by an overgrowth of the yeast Malassezia, not a bacterial infection.
- Topical agents such as ketoconazole and selenium sulfide cure most cases within 1-2 weeks.
- Oral antifungal courses are reserved for extensive or recurrent disease and show cure rates above 90%.
- Adherence to the full treatment duration and proper skin care are the biggest predictors of lasting success.
- Recurrence is common; preventive maintenance with low‑dose shampoos can keep the yeast in check.
What Is Tinea Versicolor?
Tinea Versicolor is a common superficial fungal infection caused by the yeast Malassezia that leads to irregularly colored patches on the skin. It affects up to 5% of the global population, with higher prevalence in warm, humid climates because the yeast thrives in oily skin. The patches can be lighter (hypopigmented) or darker (hyperpigmented) than surrounding skin and often appear on the trunk, shoulders, and upper arms. Although the condition is not contagious or dangerous, many people seek treatment for cosmetic reasons.
How Antifungal Medications Work
Antifungal medication targets the cell membrane of fungi, disrupting the synthesis of ergosterol, a key component that maintains fungal cell integrity. By weakening the cell wall, the drug either kills the organism (fungicidal) or stops it from growing (fungistatic). For tinea versicolor, the goal is to reduce the yeast population on the skin surface and in the deeper layers of the stratum corneum.

Topical Treatments: First‑Line Options
Topical agents are the go‑to choice for mild to moderate cases because they act directly where the yeast lives and have minimal systemic side effects. Below are the most widely used creams, lotions, and shampoos.
- Ketoconazole an azole antifungal that blocks ergosterol synthesis, available as 2% cream or 1% shampoo. Clinical studies show a 70-85% clearance rate after a 2‑week course.
- Selenium sulfide a selenium‑based antifungal found in 2.5% shampoo, works by producing free radicals that damage fungal cells. Often used twice weekly for four weeks, it clears up to 80% of lesions.
- Clotrimazole a broad‑spectrum azole cream (1%) applied twice daily, effective in about 65% of patients after 2-3 weeks.
- Terbinafine an allylamine that interferes with fungal cell wall formation, used as a 1% cream for 1-2 weeks, cure rates around 70%.
For best results, apply the medication to clean, dry skin and massage gently until fully absorbed. Re‑apply according to the product label, typically once or twice daily.
Oral Treatments: When Topicals Aren’t Enough
Systemic therapy is indicated for extensive disease covering large body areas, persistent recurrence despite topical use, or when rapid clearance is required (e.g., before a wedding or vacation).
- Itraconazole a triazole taken as 200mg once daily for 5-7 days, achieving cure rates above 90% in clinical trials. It is liver‑metabolized, so baseline liver function tests are recommended.
- Fluconazole a once‑weekly dose of 300mg for 2-4 weeks, useful for patients who cannot tolerate azole creams; studies report 85-95% effectiveness.
Oral regimens are short‑term, but patients should avoid alcohol and be aware of possible drug interactions, especially with statins or certain anti‑epileptics.
Comparing Effectiveness: Topical vs. Oral
| Medication | Formulation | Typical Cure Rate | Treatment Duration | Common Side Effects | Cost (AU$) |
|---|---|---|---|---|---|
| Ketoconazole | 2% cream / 1% shampoo | 70-85% | 2weeks | Skin irritation, mild burning | 15-25 |
| Selenium sulfide | 2.5% shampoo | 75-80% | 4weeks (twice‑weekly) | Dryness, odor | 10-18 |
| Clotrimazole | 1% cream | 60-70% | 2-3weeks | Itching, redness | 12-20 |
| Terbinafine | 1% cream | 68-75% | 1-2weeks | Rare rash | 20-30 |
| Itraconazole | Oral 200mg | 90-95% | 5-7days | Headache, GI upset, liver enzyme rise | 40-70 |
| Fluconazole | Oral 300mg | 85-95% | 2-4weeks (once weekly) | Nausea, rash | 35-60 |
From the table you can see that oral agents deliver the highest clearance rates but come with higher cost and systemic risk. Topicals are cheaper and safer for most patients, yet they require strict adherence to the application schedule.
Factors That Influence Treatment Success
Even the most potent medication can fail if other variables aren’t addressed. The following factors often tip the balance between cure and recurrence:
- Adherence: Skipping doses or stopping early lets the yeast rebound.
- Skin Oiliness: Excess sebum provides a nutrient‑rich environment for Malassezia, so patients with oily skin may need longer courses.
- Environmental Conditions: Hot, humid climates and excessive sweating increase relapse risk.
- Concurrent Skin Conditions: Eczema or psoriasis can alter the barrier function, making clearance harder.
- Genetic Pigmentation: Darker skin types may notice lingering hypopigmentation even after the fungus is gone.
Practical Tips for Using Antifungal Medications
- Clean the affected area with a gentle, non‑oil‑based cleanser before applying any cream or lotion.
- Apply a thin layer of the topical agent, rubbing in until fully absorbed; for shampoos, leave the lather on the scalp and torso for 5-10minutes before rinsing.
- Continue treatment for at least 5‑7days after lesions disappear to eradicate residual yeast.
- Wear breathable fabrics and avoid tight, synthetic clothing that traps heat.
- Consider a maintenance routine: once the infection clears, use a 1% selenium sulfide shampoo once a week for three months to keep the yeast in check.
- If you notice worsening redness, swelling, or systemic symptoms (fever, joint pain), stop the medication and see a dermatologist promptly.
When to Seek Professional Help
Most cases respond to over‑the‑counter shampoos, but you should schedule a doctor visit if:
- Lesions cover more than 30% of the body surface.
- Standard topicals fail after two full courses.
- You have liver disease, are pregnant, or are on medications that might interact with oral azoles.
- There is uncertainty about the diagnosis (e.g., it could be pityriasis rosea or vitiligo).
Frequently Asked Questions
Can tinea versicolor disappear on its own?
Yes, the yeast can balance out without treatment, but patches often return when the skin gets oily or sweaty. Leaving it untreated may also make the discoloration more noticeable.
Is it safe to use selenium sulfide shampoo daily?
Daily use is generally unnecessary and may cause scalp irritation. Most guidelines recommend twice a week during the active phase, then once weekly for maintenance.
Do oral antifungals affect birth control pills?
Itraconazole can reduce the effectiveness of hormonal contraceptives. Discuss alternative birth control methods with your doctor before starting an oral course.
How long does it take for skin color to return to normal after the fungus is cleared?
Pigment normalization can take several weeks to months, depending on skin type and the extent of the infection. Sun protection speeds up recovery by preventing further discoloration.
Can I use over‑the‑counter antifungal creams for tinea versicolor?
OTC products that contain ketoconazole or selenium sulfide are effective for mild cases. If there’s no improvement after two weeks, see a dermatologist for prescription‑strength options.


Comments (20)
kevin tarp
I’ve found that sticking to the recommended two‑week course of ketoconazole cream usually clears mild patches. Skipping doses often leads to relapse, so consistency is key.
ravi kumar
Look, the fact that you’re even mentioning “consistency” shows you haven’t seen the real power of a proper oral regimen. In my experience, a short burst of itraconazole wipes out even the stubborn patches your “topicals” can’t touch. Sure, liver tests are a hassle, but if you’re serious about clearing up, you pay the price. Also, don’t forget that humidity in our region makes the fungus thrive, so the oral route is practically mandatory.
SandraAnn Clark
Honestly, most over‑the‑counter shampoos just wash away the color, not the yeast.
Rex Wang
That’s a fair point-if you stop at the surface, the fungus can bounce right back; you really need to let the treatment sit for a few minutes before rinsing!!
mark Lapardin
From a pharmacological perspective, the azole class-specifically ketoconazole-exerts its antifungal effect by inhibiting the lanosterol 14α‑demethylase enzyme, thereby disrupting ergosterol synthesis in the fungal cell membrane. This mechanism underlies the observed 70‑85 % clearance rates in controlled trials when applied twice daily for the full two‑week protocol. Moreover, adherence to the dosing schedule mitigates the risk of sub‑therapeutic exposure, which can otherwise select for resistant Malassezia strains.
Barry Singleton
While the enzymatic inhibition pathway is well‑documented, real‑world data suggest that patient compliance drops precipitously beyond the first week, especially when mild irritation occurs. Consequently, the theoretical efficacy translates to a lower pragmatic success rate, unless clinicians emphasize proactive skin‑care adjuncts.
Javier Garcia
Recurrence tends to spike when only topical agents are used without maintenance shampoo.
christian quituisaca
Great observation-maintenance with a weekly selenium sulfide rinse can keep the yeast in check and dramatically cut down on flare‑ups, especially during humid summer months.
Donnella Creppel
Well, let’s be real here; the whole “topical‑only” hype is just pharma‑driven marketing fluff-nothing beats a systemic approach in the long run, okay?
Jarod Wooden
One could argue that reducing a complex mycological ecosystem to a binary “systemic vs. topical” dichotomy oversimplifies the nuanced interplay of host sebum, ambient humidity, and genetic pigment variation, thereby ignoring the multifactorial nature of dermatologic homeostasis.
lee charlie
Sticking with the full course really does the trick, and staying positive helps the skin heal faster.
Greg DiMedio
Yeah, because optimism is the secret ingredient that fights fungus, right?
Badal Patel
Esteemed readers, the discourse surrounding the therapeutic hierarchy for tinea versicolor merits a scrupulous examination. Firstly, the etiological agent, Malassezia spp., exhibits a proclivity for lipid‑rich environments, thereby rendering oily dermal substrates a fertile ground for proliferation. Secondly, the pharmacodynamics of azole agents such as ketoconazole involve the inhibition of the cytochrome P450‑dependent enzyme 14α‑demethylase, culminating in impaired ergosterol synthesis. Thirdly, clinical investigations have documented a variable efficacy spectrum, with topical formulations achieving cure rates ranging from seventy to eighty‑five percent when applied meticulously. Fourthly, oral triazoles, notably itraconazole, demonstrate superior clearance percentages-often exceeding ninety percent-albeit at the expense of hepatic monitoring. Fifthly, patient adherence emerges as the pivotal determinant of therapeutic success; premature discontinuation invariably predisposes to relapse. Sixthly, the sociocultural context, particularly in humid climes, augments the recurrence probability, necessitating prophylactic regimens. Seventhly, maintenance strategies, such as intermittent selenium sulfide shampoo application, have been substantiated to attenuate re‑colonization. Eighthly, the cost‑benefit analysis must weigh the financial burden of oral agents against the potential for expedited resolution. Ninthly, adverse effect profiles differ markedly; topical agents primarily incite localized irritation, whereas systemic agents may engender hepatotoxicity and drug interactions. Tenthly, the clinician’s role encompasses patient education regarding the importance of completing the prescribed course. Eleventhly, diagnostic certainty should be affirmed via Wood’s lamp examination when ambiguity persists. Twelfthly, emerging data on novel agents, including luliconazole, suggest promising efficacy with minimal systemic exposure. Thirteenthly, interdisciplinary collaboration with dermatopathology can elucidate atypical presentations. Fourteenthly, adherence monitoring tools, such as treatment diaries, enhance compliance. Fifteenthly, in summation, a judicious, individualized approach-balancing severity, patient comorbidities, and lifestyle factors-optimally harnesses the therapeutic arsenal against tinea versicolor.
KIRAN nadarla
Your comprehensive outline is commendable; however, the omission of quantitative relapse statistics after maintenance therapy is a notable gap. Incorporating a meta‑analysis of recurrence rates would strengthen the recommendation hierarchy.
Kara Guilbert
Honestly, people who ignore liver function tests before taking oral antifungals are just being reckless.
Sonia Michelle
While safety is paramount, it’s also essential to recognize that many patients are unaware of the need for baseline labs, so clinicians should proactively discuss these precautions.
Neil Collette
Let’s cut the fluff-if you’re not measuring your liver enzymes, you might as well be playing Russian roulette with your health, and that’s on top of the embarrassing patches on your back.
James Lee
Sure, because every dermatologist loves a dramatic warning that sounds like a horror movie trailer.
Dennis Scholing
In practice, establishing a collaborative dialogue with patients-explaining the rationale behind topical versus oral choices-fosters trust and improves adherence to the treatment plan.
Kasey Lauren
Sounds good! I’ll definitely talk to my doc about the best option for me.