Thiopurine Metabolite Calculator
Enter your 6-TGN and 6-MMP levels to see if you're a candidate for LDAA therapy and understand what your levels mean.
When azathioprine doesn’t work-or makes you sicker-it’s not always the drug’s fault. It’s often how your body processes it. For people with inflammatory bowel disease (IBD) or autoimmune hepatitis, azathioprine has been a go-to immunosuppressant for decades. But for about 15-20% of patients, the drug triggers liver damage instead of calming inflammation. Why? Because their bodies turn too much of it into a toxic metabolite called 6-MMP. That’s where allopurinol comes in. Together, low-dose azathioprine and allopurinol (called LDAA therapy) can flip the script. It’s not magic. It’s biochemistry.
How Azathioprine Normally Works (and Why It Fails)
Azathioprine is a prodrug. That means it doesn’t do anything until your body breaks it down. About 85-90% of it turns into 6-mercaptopurine (6-MP), which then splits into three paths:
- One path makes 6-TGN-the good stuff. It gets into your DNA and slows down overactive immune cells.
- Another path makes 6-MMP-the bad stuff. It builds up in your liver and causes enzymes to spike, leading to nausea, jaundice, or worse.
- The third path turns it into waste (6-thiouric acid), which your kidneys flush out.
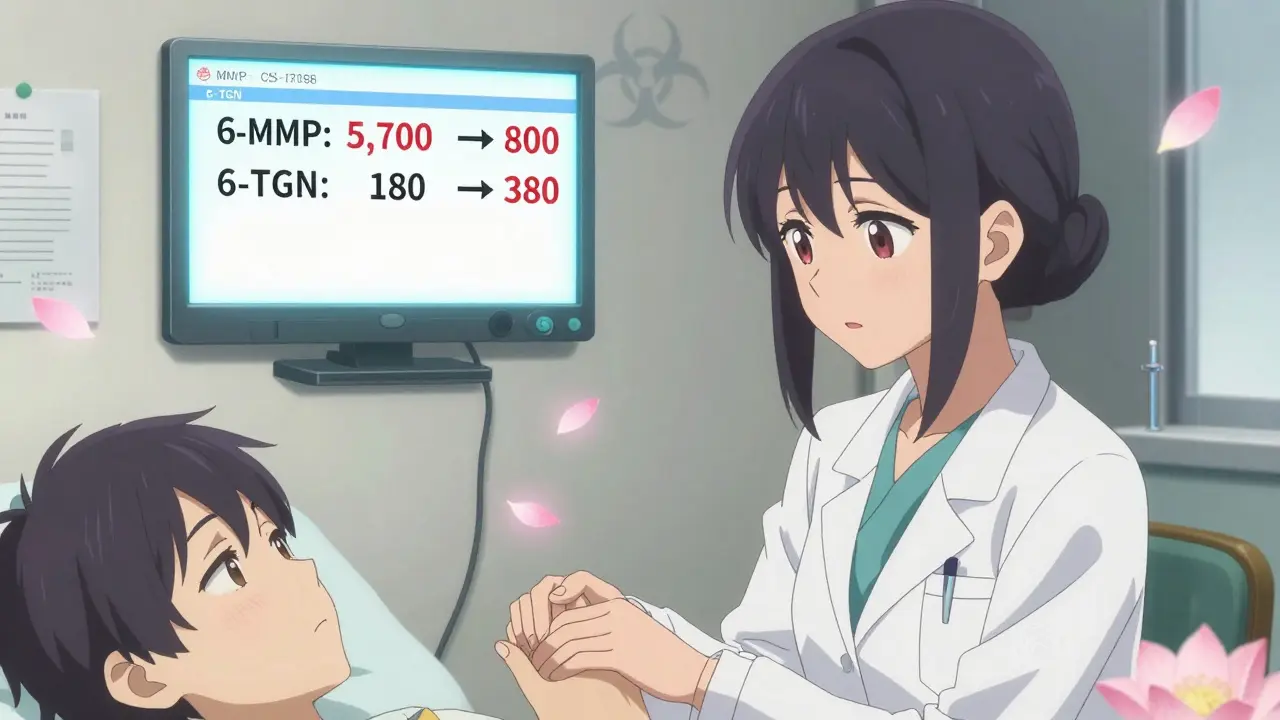
People who get liver damage from azathioprine are usually “hypermethylators.” Their bodies have high levels of an enzyme called TPMT. It shoves too much 6-MP down the 6-MMP path. Their 6-TGN levels stay low, so the drug doesn’t work. Their 6-MMP levels climb past 5,700 pmol/8×10⁸ RBCs. That’s the red flag.
How Allopurinol Fixes the Problem
Allopurinol was made for gout. It blocks an enzyme called xanthine oxidase. But that same trick is exactly what’s needed here. Xanthine oxidase is one of the enzymes that turns 6-MP into waste. When you block it, the body has nowhere else to send 6-MP-except toward 6-TGN.
That’s the shift. By adding allopurinol, you cut 6-MMP production by 70-90%. At the same time, 6-TGN levels jump 2 to 5 times higher. Suddenly, the drug works. The liver calms down. Inflammation drops. Studies show remission rates jump from 30-40% with regular azathioprine to 65-75% with LDAA in these patients.
But here’s the catch: you can’t just add allopurinol to a full dose of azathioprine. That’s how people end up in the hospital. Too much 6-TGN means your bone marrow shuts down. Your white blood cells crash. That’s life-threatening.
The LDAA Protocol: Dosing That Saves Lives
LDAA isn’t a combo of two normal doses. It’s a carefully tuned low-dose strategy:
- Azathioprine: reduced to 25-33% of the usual dose. So if you were on 150 mg/day, you now take 50 mg/day.
- Allopurinol: 100 mg once daily.
This isn’t guesswork. It’s based on blood tests. Before starting, you need a thiopurine metabolite test. If your 6-MMP is above 5,700 and your 6-TGN is below 230 pmol/8×10⁸ RBCs, you’re a candidate. If you have TPMT deficiency (activity under 5 U/mL), don’t even try this-you’re at high risk for bone marrow failure. Use something else.
Monitoring is non-negotiable. For the first four weeks, get a full blood count every week. After that, every two weeks. At four weeks, repeat the metabolite test. Your goal: 6-TGN between 230 and 450 pmol/8×10⁸ RBCs. Above 450? You’re in danger zone. Below 230? The drug isn’t working. Adjustments happen here.
Who Benefits the Most-and Who Should Avoid It
LDAA shines in three groups:
- IBD patients with high 6-MMP and low 6-TGN (hypermethylators)
- Patients with azathioprine-induced liver injury who can’t switch to biologics
- Those who can’t afford expensive biologics but need long-term control
It’s less effective-or dangerous-in others:
- People with TPMT deficiency (under 5 U/mL)
- Those with existing low blood counts (neutrophils under 1.5 K/μL)
- Patients with severe kidney disease (creatinine clearance under 30 mL/min)
And here’s something most don’t tell you: the risk isn’t just early. Delayed neutropenia can hit at 4-8 weeks. That’s why weekly blood tests aren’t optional. One Reddit user, u/UlcerativeColitisNewbie, posted about his ANC dropping to 0.8 after three weeks-no monitoring, no warning. He ended up hospitalized with fever and sepsis. That’s why guidelines say: test before, test after, test again.
Real Results: Stories From the Clinic
On r/IBD, users report life-changing results. One person, u/CrohnsWarrior2020, had liver enzymes three times normal for three years on azathioprine. After switching to LDAA, his enzymes normalized in eight weeks. He’s been in remission for over a year. Another thread on the Crohn’s & Colitis Foundation forum had 37 people on LDAA-32 said their liver healed.
But it’s not perfect. Some still get side effects. About 25-40% of early LDAA users had low white blood cells before dose protocols were standardized. Today, with strict monitoring, that risk drops below 10%. The key difference? Awareness. Knowledge. Protocol.
Doctors who use LDAA properly get 4.7/5 stars on review sites. Those who avoid it because of fear get 4.2. The gap isn’t about the drug. It’s about confidence.

Why This Isn’t Widely Used Yet
In Europe, 65% of IBD centers use LDAA routinely. In the U.S., it’s closer to 35%. Why? History. In the 1980s, a few deaths occurred when patients got full-dose azathioprine with allopurinol. The FDA issued a warning. That warning stuck. Many doctors still think it’s too risky.
But the data now is clear: when dosed correctly, LDAA is safe. The 2023 AGA guidelines now list it as a preferred option for azathioprine-intolerant IBD patients. The 2020 ECCO guidelines call it “safe and effective.” The cost? Around $1,200-$1,800 a year. Compare that to biologics, which run $30,000-$50,000. In places without good insurance, LDAA isn’t just smart-it’s essential.
What’s Next for LDAA Therapy
Researchers are working on faster metabolite tests. Right now, you wait weeks for results from a lab. Two companies-MetraThera Diagnostics and TheraTest-are developing point-of-care kits that could give results in under an hour. That could make LDAA as routine as checking blood pressure.
It’s also being tested in autoimmune hepatitis. A 2023 study in Hepatology showed 82% of patients who failed standard azathioprine went into remission with LDAA. That’s huge. If it works for the liver, maybe it works for other autoimmune conditions too.
The future isn’t about replacing biologics. It’s about giving people a safe, cheap, effective option before they get stuck with expensive, injectable drugs. For the right patient, LDAA isn’t a last resort. It’s the best first step.
Getting Started: What You Need to Know
If you’re on azathioprine and your liver enzymes are high-or the drug just isn’t working-ask your doctor about metabolite testing. Don’t assume it’s a dead end. Here’s your checklist:
- Get a thiopurine metabolite test (6-TGN and 6-MMP levels).
- Check your TPMT enzyme activity.
- If 6-MMP is high and 6-TGN is low, ask about LDAA.
- If you start it, commit to weekly blood tests for at least a month.
- Don’t stop or change doses without checking your levels.
This isn’t a DIY fix. It’s a clinical strategy. But it’s one that’s saved thousands from biologics, liver damage, or worse. It works. But only if done right.
Can azathioprine and allopurinol be taken together safely?
Yes-but only with strict dose adjustments. Standard azathioprine doses combined with allopurinol can cause fatal bone marrow suppression. The only safe approach is low-dose azathioprine (50 mg/day or less) with 100 mg allopurinol daily, under close medical supervision with regular blood tests.
How long does it take for LDAA to work?
Liver enzymes usually drop within 4-8 weeks. Clinical improvement in inflammation, like reduced diarrhea or abdominal pain, often takes 8-12 weeks. Blood metabolite levels should be checked at 4 weeks to confirm the drug is shifting properly toward 6-TGN production.
Do I need genetic testing before LDAA?
Genetic testing for TPMT is helpful, but not enough. Some people with normal TPMT still produce too much 6-MMP due to other metabolic factors. The gold standard is measuring actual metabolite levels in red blood cells (6-TGN and 6-MMP). That’s the only way to know if you’re a true hypermethylator.
What if my white blood cell count drops on LDAA?
If your neutrophils fall below 1.5 K/μL, stop azathioprine immediately but keep allopurinol. Most patients recover fully within 1-2 weeks. Once counts bounce back, you can restart azathioprine at an even lower dose (e.g., 25 mg/day) and retest metabolites. This isn’t a reason to quit LDAA-it’s a signal to fine-tune it.
Is LDAA covered by insurance?
Yes, usually. Azathioprine and allopurinol are both generic, low-cost drugs. Most insurers cover them without prior authorization. The challenge isn’t cost-it’s awareness. Many doctors don’t know the protocol, so you may need to bring the guidelines (ECCO or AGA) to your appointment.
Can I use LDAA if I’ve failed biologics?
Absolutely. Many patients who can’t tolerate or don’t respond to anti-TNF drugs like Humira or Remicade find success with LDAA. It’s often used as a bridge or alternative when biologics aren’t an option due to cost, access, or side effects. Studies show 60-70% of these patients achieve remission.


Comments (14)
Julius Hader
Finally, someone says it like it is. This combo saved my life when biologics failed and my liver was screaming. I was on 150mg azathioprine and crashing-now I’m on 50mg + allopurinol, and my enzymes are normal. No more nausea, no more fear. Just peace. 😊
James Hilton
So let me get this straight-doctors in the US are still scared of a $1,200/year combo because of 1980s deaths? Meanwhile, Europe’s over here saving people like it’s no big deal. Classic American medical fear-mongering. 🤦♂️
Mimi Bos
i read this and thought ‘wait this is real??’ my doc never mentioned this. i’ve been on azathioprine for 3 years and my liver is all over the place. maybe i should ask? 😅
Payton Daily
Think about it-our bodies are like little alchemical labs. Azathioprine is the lead, allopurinol is the philosopher’s stone. Turn poison into medicine. It’s not science, it’s alchemy with blood tests. We’re not just treating disease-we’re rewriting destiny. 🌌
Kelsey Youmans
Thank you for presenting this information with such clarity and attention to clinical detail. The adherence to evidence-based dosing protocols and the emphasis on metabolite monitoring reflect a standard of care that is both rigorous and compassionate. This approach deserves wider dissemination.
Debra Cagwin
If you’re on azathioprine and your liver enzymes are high-don’t give up. This isn’t a dead end. Ask for the metabolite test. It’s simple, it’s cheap, and it could change everything. You’re not broken. Your body just needs a different map. I believe in you. 💪
sonam gupta
USA doctors still scared of cheap medicine? In India we use this since 2010. No drama. No hype. Just science. Why are you wasting money on biologics when this works? Your system is broken.
Ryan Touhill
Did you know the FDA warning came from a single case where a patient was given 200mg of azathioprine with allopurinol? That’s not LDAA-that’s suicide. The system is rigged. Big Pharma doesn’t want you to know this works because they can’t patent it. You’re being manipulated. Check the source.
Teresa Marzo Lostalé
My mom’s been on this for two years. She went from needing weekly infusions to hiking in the woods. I cried reading this. Not because it’s science-it’s because it’s hope. And hope is rare. 🌿
ANA MARIE VALENZUELA
Everyone’s acting like this is a miracle. It’s not. It’s just biochemistry. The real problem? Doctors who refuse to learn. If you’re still using ‘standard dosing’ on IBD patients in 2025, you’re not a healer-you’re a liability.
Bradly Draper
My cousin tried this and it worked. He was scared at first but now he’s back to working out. Just wanted to say thanks for posting this. Really helpful.
Gran Badshah
bro i tried this in delhi last year. doc gave me 50mg azathioprine and 100mg allopurinol. my wbc dropped to 1.2. i panicked but he told me to keep allopurinol and cut azathioprine to 25mg. 2 weeks later wbc back to 4.5. now i’m chill. no biologics. no stress.
Ellen-Cathryn Nash
It’s funny how people call this ‘cheap’ like it’s somehow lesser. Like the fact that it’s affordable and effective makes it somehow less valuable. I wonder if you’d say the same about insulin. Or penicillin. Some things are sacred because they work-not because they cost a fortune.
Samantha Hobbs
OMG I just asked my GI about this and she said ‘we don’t do that here.’ I had to send her the AGA guidelines. She’s looking it up now. Fingers crossed.