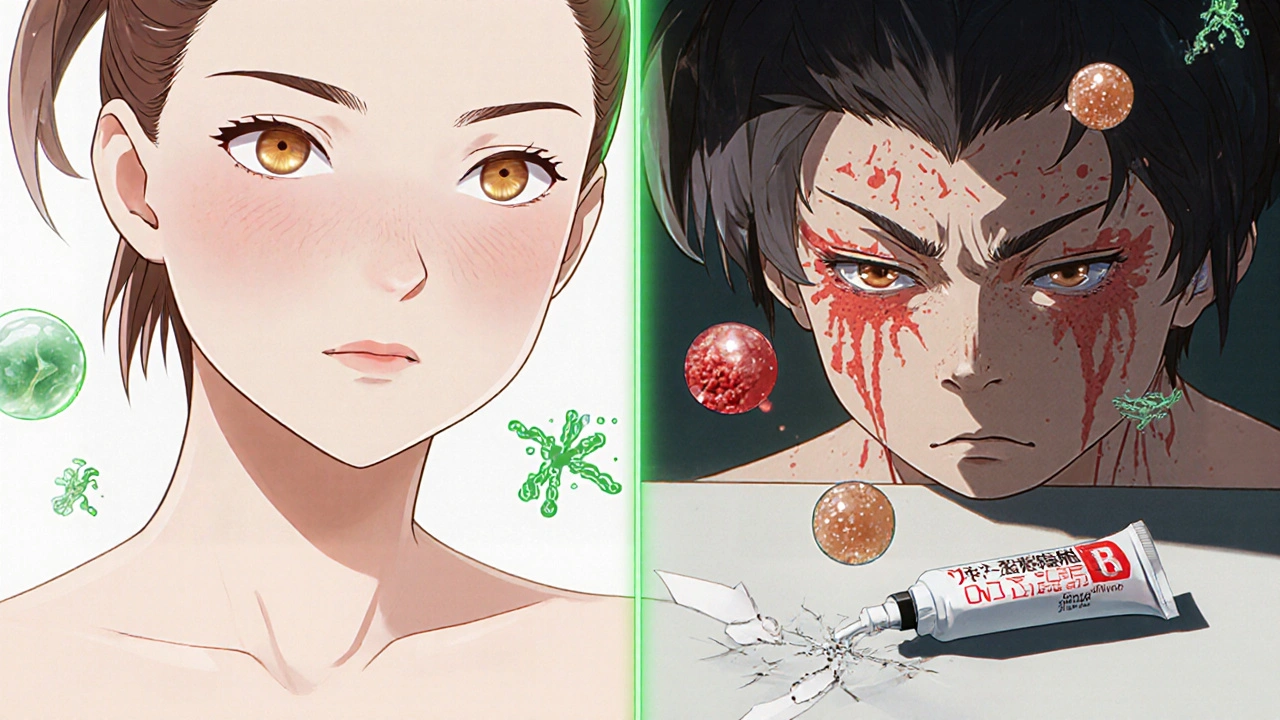
Most people reach for benzoyl peroxide or salicylic acid when acne flares up. But what if someone accidentally uses a steroid cream like betamethasone on their face? It might seem like a quick fix for redness or irritation-but it could be making things a lot worse.
What is betamethasone?
Betamethasone is a strong topical corticosteroid. It’s commonly prescribed for eczema, psoriasis, allergic rashes, and other inflammatory skin conditions. It works by calming down the immune system’s response in the skin, which reduces swelling, itching, and redness. You’ll find it in creams, ointments, and lotions under brand names like Betnovate or Celestone.
But here’s the catch: it’s not meant for acne. Acne isn’t caused by inflammation alone-it’s driven by clogged pores, excess oil, bacteria (Cutibacterium acnes), and hormones. Betamethasone doesn’t touch any of those root causes. Instead, it masks symptoms while letting the real problem grow underneath.
Why people try betamethasone for acne
It’s not unusual to see someone use a steroid cream on acne by accident-or on purpose. Maybe they had a bad reaction to a facial product and their skin turned red and angry. They grabbed the leftover eczema cream from the bathroom cabinet. Or maybe they saw a social media post claiming steroids "clear acne fast."
At first, it might seem to work. The redness fades. The bumps look less swollen. For a few days, the skin looks smoother. That’s because betamethasone suppresses inflammation. But that’s where the benefit ends.
How betamethasone makes acne worse
Using betamethasone on acne can trigger a chain reaction that leads to worse breakouts over time. Here’s how:
- It thickens the skin. Steroids reduce cell turnover, which means dead skin cells don’t shed properly. These pile up and clog pores-exactly what causes acne.
- It increases oil production. Studies show that topical corticosteroids can stimulate sebaceous glands. More oil = more clogged pores = more acne.
- It weakens the skin’s defenses. By suppressing local immunity, betamethasone lets acne-causing bacteria multiply unchecked.
- It causes steroid-induced acne. This isn’t regular acne. It looks like small, uniform red bumps (papules) or pus-filled pimples (pustules), often around the mouth, chin, or forehead. It’s called steroid acne, and it’s a known side effect.
Some people develop perioral dermatitis after using steroid creams on their face. This looks like a red, bumpy rash around the mouth and nose-often mistaken for acne. It’s actually a reaction to the steroid itself and can take months to clear up once you stop using it.
What the research says
A 2020 study in the Journal of the American Academy of Dermatology tracked 89 patients who developed acne-like rashes after using topical steroids on their face. Nearly all cases cleared up only after stopping the steroid-and most required a different treatment, like antibiotics or non-steroidal anti-inflammatories, to fully recover.
The American Academy of Dermatology warns that long-term use of potent steroids like betamethasone on the face can cause thinning skin, visible blood vessels, and permanent textural changes. Acne is just one of many risks.
What to use instead
If you have acne, stick with proven treatments:
- Benzoyl peroxide kills bacteria and unclogs pores.
- Salicylic acid exfoliates inside pores to prevent blockages.
- Retinoids (like adapalene) speed up skin cell turnover and reduce inflammation long-term.
- Topical antibiotics (like clindamycin) target acne bacteria without suppressing immunity.
- Oral medications like spironolactone or isotretinoin for moderate to severe cases-only under a doctor’s care.
For sudden redness or irritation, try a gentle, fragrance-free moisturizer with ceramides or niacinamide. These soothe without clogging pores or suppressing your skin’s natural defenses.

What to do if you’ve already used betamethasone on acne
If you’ve applied betamethasone to your face for acne, stop immediately. Don’t just taper off-quit cold turkey. Continuing to use it will only deepen the problem.
Expect a flare-up in the first 1-3 weeks after stopping. This is called steroid rebound. Your skin is overreacting because it’s been suppressed. It’s not a sign the treatment worked-it’s a sign your skin is trying to reset.
During this phase:
- Avoid harsh scrubs or alcohol-based toners-they’ll irritate more.
- Use a mild cleanser and a simple moisturizer.
- Apply a cool compress if your skin feels hot or burning.
- See a dermatologist if breakouts don’t improve after 4-6 weeks.
Don’t panic. Your skin can recover. But it takes time. Most people see improvement within 2-3 months, though some cases take longer.
When to see a doctor
See a dermatologist if:
- Your acne worsens after using any steroid cream.
- You notice thinning skin, stretch marks, or visible veins on your face.
- You develop a rash around your mouth that won’t go away.
- Over-the-counter acne treatments haven’t helped after 8 weeks.
Doctors can prescribe non-steroid options that actually treat the root causes of acne-not just hide the symptoms.
Final takeaway
Betamethasone has no place in acne treatment. It doesn’t cure acne-it hides it, then makes it worse. What looks like a quick fix is actually a trap. The temporary calm it brings is followed by a bigger breakout, harder-to-treat skin damage, and longer recovery.
Acne needs targeted care, not immune suppression. Stick to treatments designed for it. Your skin will thank you.
Can betamethasone clear acne?
No, betamethasone cannot clear acne. It may temporarily reduce redness and swelling, but it doesn’t address the root causes like clogged pores, excess oil, or bacteria. In fact, it often makes acne worse by thickening the skin, increasing oil production, and weakening the skin’s natural defenses.
Is steroid acne the same as regular acne?
No, steroid acne is different. It usually appears as small, uniform red bumps or pustules, often around the mouth, chin, or forehead. It develops because steroids disrupt normal skin function, not because of hormonal changes or bacteria alone. It doesn’t respond to typical acne treatments and requires stopping the steroid first.
How long does it take for skin to recover after stopping betamethasone?
Recovery varies. Most people notice improvement in 2-6 weeks, but full healing can take 2-6 months. The first 1-3 weeks after stopping often involve a flare-up called steroid rebound. Patience and gentle skincare are key. If no improvement occurs after 8 weeks, see a dermatologist.
Can I use betamethasone on acne scars?
No. Betamethasone does not treat acne scars. It can actually thin the skin and make scarring worse over time. For scars, treatments like retinoids, chemical peels, microneedling, or laser therapy are more effective-and safe when guided by a dermatologist.
What’s the safest way to treat facial redness from acne?
Use gentle, non-steroid products with niacinamide, azelaic acid, or centella asiatica. These reduce redness and inflammation without suppressing your skin’s natural healing. Avoid anything with alcohol, fragrance, or steroids. Moisturizing with ceramides also helps repair the skin barrier.


Comments (10)
Erika Puhan
Let’s be real-using betamethasone for acne is like pouring gasoline on a smoldering ember and calling it a fireplace. The temporary reduction in redness is just the universe giving you a false sense of control. The real damage? It’s systemic. Steroids disrupt the follicular keratinization cascade, increase sebum viscosity, and suppress local IL-1β and TNF-α signaling-all of which are critical for microbial homeostasis. You’re not treating acne; you’re engineering a microbiome collapse. And when you stop? Welcome to steroid rebound syndrome, which isn’t even a real diagnosis in the DSM but should be. Your skin isn’t ‘reacting’-it’s screaming for help.
And yet, people still do it. Because convenience > competence. Because Instagram dermatologists don’t mention the 6-month recovery window. Because we’ve normalized quick fixes over sustainable healing. Sad.
Pro tip: If you’re using a steroid cream on your face without a prescription, you’re not skincare-ing-you’re self-sabotaging.
Edward Weaver
LMAO Americans think they can just slap steroid cream on their face and call it a day. We got real medicine in the US-like retinoids and antibiotics-but no, some dude’s cousin’s friend saw a TikTok and now his whole chin looks like a red swamp. Betamethasone ain’t magic. It’s a trap. And if you’re dumb enough to use it on acne, you deserve every breakout you get. Get a real dermatologist, not some influencer with 3 followers and a bottle of Betnovate.
Also, stop using ‘natural’ stuff. Your skin doesn’t need tea tree oil and affirmations. It needs science.
Lexi Brinkley
OMG YES 😭 I did this. Used my mom’s eczema cream on a zit. Thought it was a miracle. Then my face turned into a red, burning mess. Like… I could feel my skin screaming. I cried. I googled. I found this post. Now I’m terrified to touch my face again. But thank you for explaining why it happened. I didn’t know it was called ‘steroid acne.’ 🥲 #SkinRecoveryJourney
Jay Wallace
Look, I get it-people want fast results. But this isn’t a 2020s skincare TikTok trend. This is dermatology. Betamethasone is a Class II corticosteroid. That means it’s potent. That means it’s dangerous on the face. That means you’re not ‘trying to help’-you’re playing Russian roulette with your epidermal barrier. And now you’re gonna need a $500 laser treatment because you thought a cream labeled ‘for eczema’ was a universal acne fix? Wow. Just wow. You didn’t need a dermatologist-you needed a basic biology class.
Alyssa Fisher
There’s something deeply human about reaching for what’s familiar when your skin is in crisis. We don’t have a language for skin distress, so we borrow tools from other conditions-like eczema creams-because they ‘work’ on redness. But acne isn’t inflammation alone. It’s a systemic dysfunction of the pilosebaceous unit. The irony? We treat symptoms like enemies, when they’re just signals. Betamethasone doesn’t heal. It silences. And silence, in biology, is never peace-it’s just waiting for the explosion.
Maybe the real question isn’t ‘why do people misuse steroids?’ but ‘why don’t we teach people how to listen to their skin?’
Alyssa Salazar
Okay but let’s talk about steroid rebound-this is REAL. I stopped using my prescription cream after 3 weeks and my face looked like a crime scene. Like, 50+ tiny pustules overnight. I thought I was healing. Turns out I was just in withdrawal. Derm told me it’s called ‘rebound acne’ and it’s a legit thing. Took me 4 months to get back to normal. I’m now obsessed with niacinamide and ceramides. If you’re using steroids on your face, STOP. And if you already did? You’re not broken-you’re just in recovery mode. Be patient. Your skin is fighting for you.
Beth Banham
I’ve seen this happen to friends. One girl used hydrocortisone for months thinking it was helping. She didn’t realize her ‘clear skin’ was a lie. When she stopped, it got worse. She cried for weeks. I just sat with her. No advice. Just presence. Skin recovery isn’t just physical-it’s emotional too. You’re not just healing pores. You’re healing shame. Be gentle with yourself. It’s okay to take time.
Brierly Davis
You got this 💪 I know it’s scary after stopping the cream-trust me, I’ve been there. But your skin isn’t broken, it’s just resetting. Stick with the gentle stuff: fragrance-free moisturizer, cool compresses, no scrubs. You’ll start seeing improvement in a few weeks. And hey-if you need someone to vent to about your ‘rebound phase,’ I’m here. You’re not alone in this. Progress > perfection. Keep going 😊
Jim Oliver
Wow. Someone actually used a steroid for acne. Shocking. Next they’ll use toothpaste as moisturizer. Or bleach as toner. You didn’t need a 1000-word essay-you needed to read the damn label. ‘For external use only. Not for face. Not for acne.’ It’s written in 12-point font. You’re not a victim. You’re a cautionary tale.
William Priest
So… betamethasone = bad. Got it. But like… why are we even talking about this? Everyone knows steroids are for eczema. Who even uses them on their face? This post feels like someone trying to make a big deal out of a dumb mistake. Also, ‘steroid acne’? Sounds like something a med student made up to sound smart. Just use benzoyl peroxide. Done. 🤷♂️