Progestin Decision Guide
Find Your Best Progestin Match
If you’ve ever opened a prescription bottle and wondered how Aygestin vs other progestins really stack up, you’re not alone. Hormonal therapy can feel like a maze of names, dosages, and side‑effects, especially when your doctor mentions alternatives without explaining why one might be a better fit for you. This guide cuts through the jargon, walks you through the science, and gives you a side‑by‑side look at the most common substitutes for Aygestin (norethindrone).
Key Takeaways
- Aygestin (norethindrone) is a third‑generation progestin mainly used for menstrual disorders, endometriosis, and hormone replacement therapy.
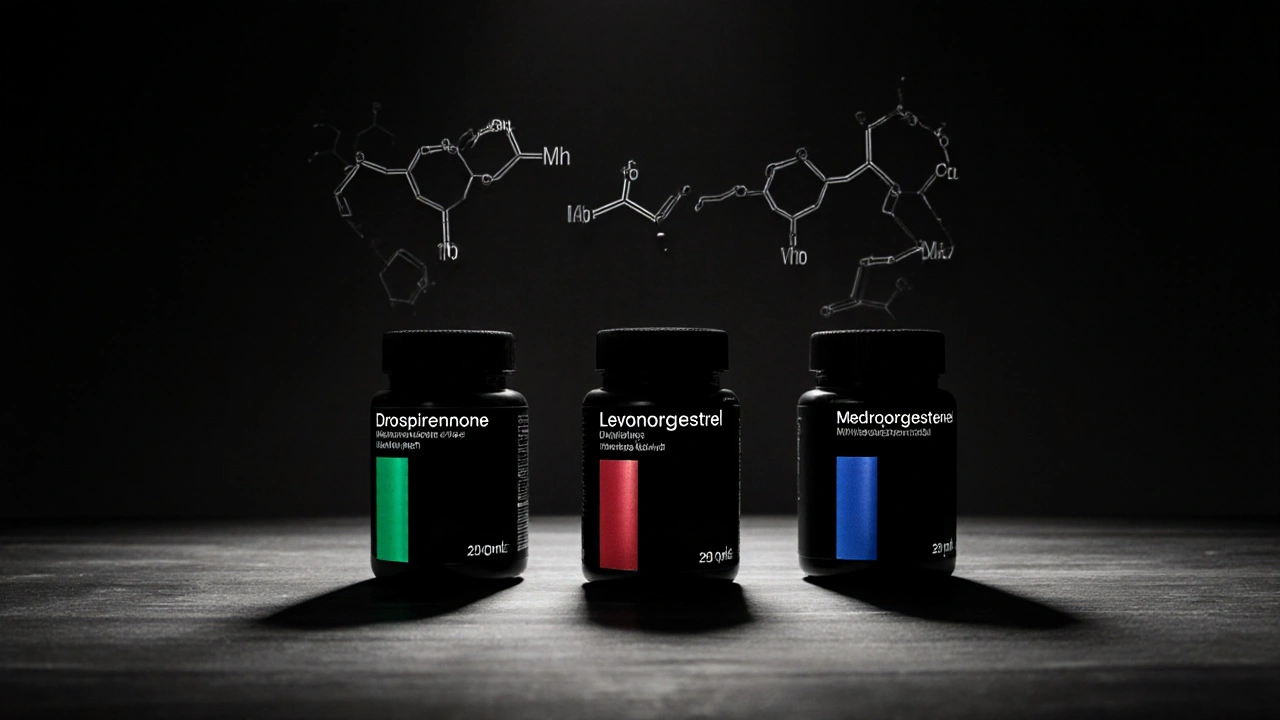
- Drospirenone and levonorgestrel are the most frequently prescribed alternatives, each with distinct metabolic profiles.
- Medroxyprogesterone acetate is a long‑acting option suited for contraception and certain cancer therapies.
- Side‑effect patterns differ: weight gain is more common with medroxyprogesterone, while drospirenone may raise potassium levels.
- Choosing the right progestin hinges on your health goals, liver function, and any existing clotting risks.
What Is Aygestin (Norethindrone)?
When it comes to hormonal therapy, Aygestin (norethindrone) is a synthetic progestin that mimics the natural hormone progesterone. Approved by the FDA in 1965, it is prescribed for a range of conditions, including abnormal uterine bleeding, endometriosis, and as part of hormone replacement therapy (HRT) for menopausal women. The typical oral dose ranges from 0.35mg to 5mg per day, depending on the indication. Key attributes of Aygestin include:
- Half‑life: Approximately 8-12hours, meaning it must be taken daily for stable blood levels.
- Receptor activity: Strong affinity for progesterone receptors, weak androgenic activity, and negligible estrogenic effect.
- Metabolism: Primarily hepatic via CYP3A4 enzymes, which can interact with common drugs like antibiotics and antifungals.
Why Look at Alternatives?
Although Aygestin works well for many, it isn’t a one‑size‑fits‑all solution. Some patients experience side‑effects such as breakthrough bleeding, mood swings, or lipid changes. Others have contraindications-like a history of blood clots-that make certain progestins riskier. That’s why doctors often consider alternatives that may provide better tolerance, longer dosing intervals, or a more favorable metabolic profile.
Top Progestin Alternatives
Below are the most common substitutes, each introduced with a brief definition and its typical clinical use.
Drospirenone is a fourth‑generation progestin with anti‑androgenic and anti‑mineralocorticoid properties. It’s found in many combined oral contraceptives (COCs) and in some HRT formulations. The anti‑mineralocorticoid effect can help reduce water retention, but it also means potassium monitoring is advised for patients taking ACE inhibitors.
Levonorgestrel is a second‑generation progestin widely used in emergency contraception, intrauterine devices (IUDs), and COCs. It has a higher androgenic activity than norethindrone, which can lead to acne or lipid changes, but its long‑acting IUD form provides up to 5years of contraception with minimal systemic exposure.
Medroxyprogesterone acetate (MPA) is a synthetic progestin with a long half‑life (up to 50days when injected). It’s commonly administered as Depo‑Provera for contraception or to treat certain cancers (e.g., endometrial carcinoma). MPA’s strong glucocorticoid activity can affect blood glucose and bone density.
Norgestrel is a first‑generation progestin often combined with estrogen in low‑dose COCs. It has lower androgenic activity than levonorgestrel but is less commonly prescribed today due to newer agents offering better side‑effect profiles.
Progesterone (bioidentical) is the naturally occurring hormone extracted from plant sources. Bioidentical compounding offers a “more natural” option, yet it suffers from poor oral bioavailability and requires micronized formulations for effectiveness.
Head‑to‑Head Comparison Table
| Attribute | Aygestin (norethindrone) | Drospirenone | Levonorgestrel | Medroxyprogesterone acetate | Progesterone (bioidentical) |
|---|---|---|---|---|---|
| Generation | Third | Fourth | Second | Second | Natural |
| Typical Use | Menstrual disorders, endometriosis, HRT | COCs, HRT (anti‑water retention) | Emergency contraception, IUD, COCs | Injectable contraception, cancer therapy | Compounded HRT |
| Androgenic Activity | Low | Very low (anti‑androgenic) | High | Moderate | None |
| Anti‑Mineralocorticoid | No | Yes | No | No | No |
| Half‑Life (oral) | 8-12h | ≈30h | ≈24h | ≈50days (injectable) | Variable, poor oral absorption |
| Common Side‑Effects | Breakthrough bleeding, mood changes | Elevated potassium, breast tenderness | Acne, weight gain | Weight gain, bone density loss | Headache, nausea |
| Contraindications | Liver disease, clotting disorders | Severe hypertension, renal disease | Smokers >35, clotting disorders | Uncontrolled diabetes, osteoporosis | Pregnancy (unless prescribed) |
How to Choose the Right Progestin for Your Situation
Picking a progestin isn’t just about brand name-it’s a decision that balances efficacy, safety, and personal tolerance. Here’s a quick decision tree you can run through with your clinician:
- Identify Your Primary Goal: Is it contraception, menstrual regulation, endometriosis relief, or menopausal symptom control?
- Assess Health Risks: Do you have a history of blood clots, hypertension, liver disease, or diabetes?
- Consider Dosing Preference: Do you want a daily pill, a monthly injection, or a long‑acting IUD?
- Review Side‑Effect Profile: Which potential side‑effects are most tolerable for you?
- Finalize with Your Provider: Use the above answers to narrow down to 1‑2 candidates and discuss monitoring plans.
For example, a non‑smoker woman in her early 30s with mild hypertension may benefit from drospirenone’s anti‑water‑retention effect, while a patient with a strong family history of osteoporosis might avoid medroxyprogesterone acetate.
Practical Tips for Managing Side‑Effects
- Track Symptoms: Keep a simple diary noting bleeding patterns, mood changes, and any weight fluctuations.
- Adjust Timing: Taking the pill at the same time each day reduces hormonal peaks that can cause breakthrough bleeding.
- Nutrition Matters: A diet rich in leafy greens and low in processed sugars can help mitigate weight gain associated with some progestins.
- Regular Labs: If you’re on drospirenone, ask for a quarterly potassium check; for medroxyprogesterone acetate, a bone density scan every two years is prudent.
Frequently Asked Questions
Can I switch from Aygestin to another progestin without a washout period?
Most clinicians recommend a short overlap of 2-3days to maintain hormonal coverage, especially when moving between progestins with different half‑lives. Your doctor will tailor the schedule based on the specific agents involved.
Is Aygestin safe for women over 50?
Aygestin can be used in menopausal hormone therapy, but the dose is usually lower (0.35mg) and combined with estrogen. Women with a history of cardiovascular disease should discuss risks with their physician.
What makes drospirenone different from norethindrone?
Drospirenone’s anti‑mineralocorticoid activity helps reduce bloating but can raise potassium levels, while norethindrone has modest androgenic activity and no anti‑mineralocorticoid effect.
How long does medroxyprogesterone acetate stay active after an injection?
A single 150mg intramuscular injection provides contraceptive effect for roughly 12‑14weeks, thanks to its long half‑life and depot formulation.
Are bioidentical progesterone creams as effective as oral progestins?
Topical bioidentical creams provide local effects but achieve lower systemic levels than oral or injectable progestins, making them less reliable for contraception or severe endometriosis.
Next Steps and Troubleshooting
After reading this comparison, the most important move is to schedule a consultation with your healthcare provider. Bring this article (or a printed copy) to discuss:
- Your specific symptom profile.
If you start a new progestin and notice persistent side‑effects beyond two menstrual cycles, ask about a dose adjustment or a switch to an alternative. Remember, hormonal therapy is highly individual-what works for your neighbor might not be optimal for you.
Bottom Line
Aygestin (norethindrone) remains a solid choice for many women, but alternatives like drospirenone, levonorgestrel, and medroxyprogesterone acetate offer distinct benefits that can better align with personal health goals. By understanding each agent’s strengths, metabolism, and side‑effect profile, you can have a focused conversation with your doctor and land on the medication that feels right for your body.


Comments (17)
Julia Grace
Aygestin is a solid go‑to for many with irregular cycles, but you gotta watch liver function. The half‑life is short so taking it at the same time daily keeps levels steady. If you’re juggling antibiotics, remember CYP3A4 can crank up metabolism, so you may need a tweak. Also, the mild androgenic side‑effects are usually okay, just keep an eye on acne. Overall it’s a decent starter before you jump to heavier stuff.
Sadie Bell
You’ve got this! Switching progestins isn’t a scary science experiment-think of it as fine‑tuning your body’s playlist. If Aygestin feels off, drospirenone can give you that anti‑bloat boost, and levonorgestrel’s long‑acting IUD is a set‑and‑forget hero. Keep tracking symptoms and share them with your doc, and you’ll land on the perfect fit!
Noah Bentley
Wow, another endless table of hormones. As if we needed a PhD to pick a pill. FYI, “medroxyprogesterone” isn’t a tongue‑twister, it’s just a long‑acting shot that can mess with your blood sugar. And yeah, “anti‑mineralocorticoid” isn’t a party trick, it actually lowers potassium loss. So pick one, stick to it, and stop overcomplicating.
Kathryn Jabek
In the grand dialectic of endocrine therapeutics, one must not merely accept the superficial allure of newer agents; a rigorous ontological appraisal reveals that Aygestin’s modest androgenic profile renders it a quintessential exemplar of balanced progestogenic activity, whereas drospirenone’s anti‑mineralocorticoid property, albeit novel, introduces iatrogenic risk of hyperkalaemia, demanding scrupulous monitoring. Consequently, the clinician’s duty extends beyond mere prescription to an ethical imperative of informed deliberation, lest we succumb to the seductive yet perilous allure of fashionable pharmacology.
Ogah John
Think of each progestin as a character in a story-Aygestin the steady protagonist, drospirenone the witty sidekick who keeps the bloating at bay, levonorgestrel the rugged hero of emergency plots, and MPA the old‑school mentor with a heavy‑handed approach. While the narrative sounds epic, the reality is simply about matching side‑effect tolerability with personal goals. If you’re chasing a smooth cycle without potassium drama, drospirenone may win; if bone density is your nemesis, steer clear of MPA. Embrace the plot twists, but keep the ending healthy.
Kelvin Murigi
Choosing the right progestin can feel like navigating a labyrinth, but breaking it down into logical steps makes the process manageable. First, clarify the primary therapeutic goal: are you seeking contraception, menstrual regulation, endometriosis relief, or menopausal symptom control? Second, compile a concise medical history that highlights clotting disorders, hypertension, liver disease, diabetes, or osteoporosis, as each condition interacts differently with specific agents. Third, consider pharmacokinetics: Aygestin’s 8‑12‑hour half‑life demands daily adherence, whereas medroxyprogesterone acetate provides a depot effect lasting up to three months after a single injection. Fourth, weigh the androgenic profile; levonorgestrel’s higher androgenic activity can exacerbate acne or affect lipid panels, while drospirenone’s anti‑androgenic and anti‑mineralocorticoid actions may reduce bloating but require potassium monitoring. Fifth, assess patient preference for dosing frequency-daily pill, monthly injection, or a multi‑year IUD-because convenience strongly influences compliance. Sixth, review side‑effect patterns: weight gain commonly follows medroxyprogesterone, while drospirenone may cause breast tenderness and mild potassium elevation. Seventh, evaluate drug‑drug interactions; Aygestin is metabolized by CYP3A4, so concurrent use of strong inducers or inhibitors can alter efficacy. Eighth, consider bone health; long‑term medroxyprogesterone use has been linked to decreased bone mineral density, necessitating periodic DEXA scans. Ninth, discuss the need for monitoring labs-potassium checks for drospirenone users on ACE inhibitors, glucose levels for those on medroxyprogesterone, and lipid panels for high‑androgen agents. Tenth, involve the patient in shared decision‑making, presenting the comparative table in plain language, and encouraging questions. Eleventh, document the chosen regimen and schedule follow‑up visits at 1‑3 month intervals to assess symptom control and adverse events. Twelfth, remain vigilant for breakthrough bleeding, mood changes, or new onset hypertension, which may signal the need for a switch. Thirteenth, if a switch becomes necessary, implement a short overlap of 2‑3 days to maintain hormonal coverage and avoid gaps. Fourteenth, educate the patient on maintaining a symptom diary to capture subtle changes over time. Finally, reinforce that while the progestin landscape seems daunting, a systematic approach rooted in individual risk factors and lifestyle preferences ultimately leads to optimal therapeutic outcomes.
ahmad matt
Honestly the whole Aygestin vs drospirenone debate is just pharma marketing fluff. Most docs just push the newest pill because it pays the bills, not because it’s objectively better. If you’re okay with a cheap generic, stick with norethindrone; don’t get swayed by fancy anti‑mineralocorticoid hype that only a handful of patients need. Bottom line: cheaper = fewer side‑effects, unless you’re allergic to cost.
kristine ayroso
Hey ladies! If you rlly wanna get your flow under control, Aygestin is a great start, but dont forget drospirenone can keep that bloat away. I tried both and felt less puffiness with drosp. Just make sure your doc checks potassium levels – its super important. Also, levonorgestrel IUD is a life saver – no daily pill, no fuss!
Ben Small
Just pick the progestin that fits your schedule.
Dylan Hilton
If you’re confused by the table, here’s a quick cheat: Aygestin = short‑acting, low androgen; Drospirenone = anti‑bloat, watch potassium; Levonorgestrel = strong androgen, great for IUD; MPA = long‑acting shot, watch weight and bone health. Hope that clears things up!
Christian Andrabado
Another endless hormone list, yet nobody mentions the real cost – constant mood swings and the feeling of being a lab rat. Stop glorifying side‑effects as if they’re badges of honor.
Chidi Anslem
In many cultures, the concept of hormone modulation is still emerging, so it’s crucial to respect patient values when discussing progestin options. While the pharmacology is universal, the perception of side‑effects like weight gain can differ, and clinicians should tailor counseling accordingly.
Holly Hayes
People cant just jump on any new pill because it sounds fancy. The real moral issue is taking responsibility for the side‑effects you might cause yourself and others, especially if you ignore regular check‑ups.
Penn Shade
Let’s get one thing straight: the superiority of a progestin isn’t determined by its brand name but by its receptor affinity and metabolic profile. If you’re still undecided after reading the table, you need a deeper dive into pharmacodynamics.
Jennifer Banash
Behold, the theater of hormonal therapy unfolds! As Aygestin takes the stage with its modest half‑life, drospirenone enters with a dramatic anti‑mineralocorticoid flourish, and levonorgestrel wields its androgenic sword. Yet behind the curtain lies the quiet menace of adverse events, awaiting the unwary. Choose wisely, lest the drama turn tragic.
Stephen Gachie
One could argue that progestins are merely extensions of our will to control nature, a Sisyphean task of balancing chemistry and desire. Yet the data show that drospirenone's anti‑mineralocorticoid effect is statistically significant, so perhaps the universe does favor subtle nuance.
Sara Spitzer
Honestly, the whole comparison feels like overkill. Most people just pick the cheapest generic and move on. No need for a PhD in pharmacology.