High blood pressure doesn’t always cause symptoms, but it’s quietly increasing your risk of heart attack, stroke, and kidney damage. That’s why doctors prescribe antihypertensive meds - not to make you feel better right away, but to keep you alive longer. Three of the most common classes are beta-blockers, ACE inhibitors, and ARBs. Each works differently, has different side effects, and fits different patients. Knowing how they compare can help you understand why your doctor chose one over another - or why you might need to switch.
How ACE Inhibitors Work - and Why So Many People Quit Them
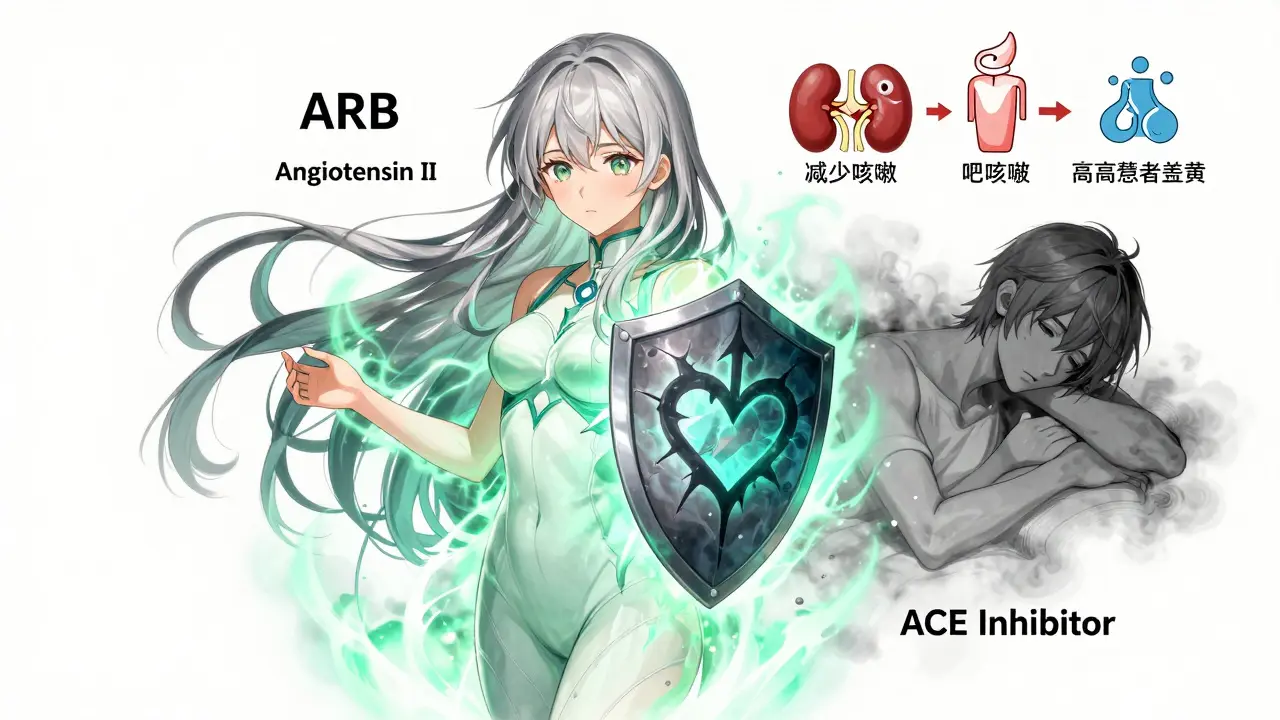
ACE inhibitors like lisinopril, enalapril, and ramipril have been the go-to for hypertension since the 1980s. They block the enzyme that turns angiotensin I into angiotensin II - a chemical that tightens blood vessels and raises blood pressure. By stopping this, they relax arteries, reduce fluid retention, and lower pressure. But here’s the catch: they also cause bradykinin to build up. That’s a harmless substance under normal conditions, but in some people, it triggers a dry, hacking cough.
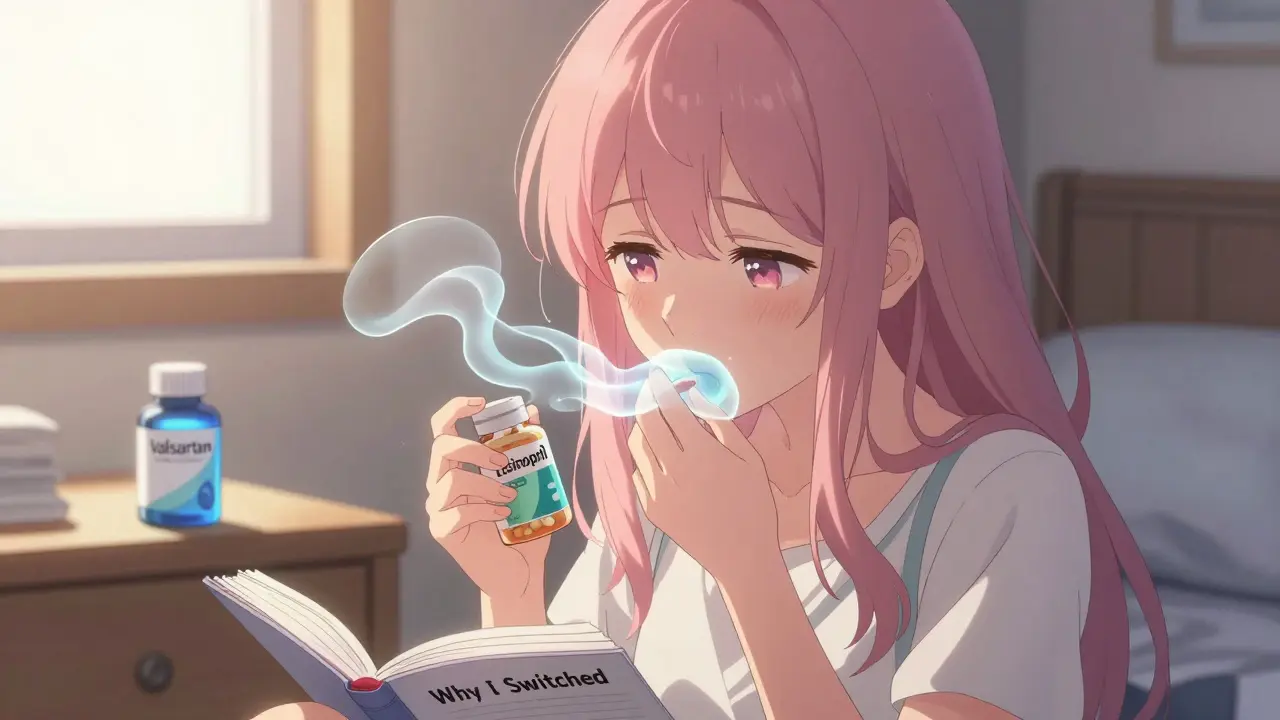
Studies show 10-20% of people on ACE inhibitors develop this cough. For some, it’s mild. For others, it’s constant, sleep-disrupting, and unbearable. One patient from Melbourne told me, "I was on lisinopril for six months. Every night, I’d wake up coughing. I thought I had a cold. Turns out, it was the pill." That’s why, according to CVS Health data from 2021, 78% of people who stop ACE inhibitors do so because of cough. And when they switch to an ARB, 89% of those cases resolve.
ACE inhibitors also carry a small but serious risk: angioedema - swelling of the face, lips, or throat. It happens in less than 1% of users, but when it does, it’s an emergency. That’s why doctors don’t prescribe them to people with a history of this reaction. Still, for patients with diabetes and kidney protein leakage (albuminuria), ACE inhibitors are the gold standard. The RENAAL trial showed they cut proteinuria by 21% more than ARBs, protecting kidney function better than any other class.
ARBs: The Tolerable Alternative
ARBs - angiotensin receptor blockers - like losartan, valsartan, and candesartan, do the same job as ACE inhibitors but without the cough. Instead of blocking the enzyme, they block the receptor that angiotensin II binds to. No bradykinin buildup. No cough. No angioedema. That’s why, in 2021, a real-world study of over 300,000 patients found ARBs had half the risk of angioedema and a 38% lower chance of cough compared to ACE inhibitors.
They’re just as effective at lowering blood pressure. In fact, ARBs reduce systolic pressure by 10-15 mmHg and diastolic by 6-8 mmHg - the same as ACE inhibitors. And while ACE inhibitors were long seen as "first-line," newer guidelines from the AHA and ESC now treat them as equals. Many cardiologists today start new patients on ARBs simply because they’re better tolerated.
One big advantage? Persistence. A 2021 analysis of 2 million patients showed 63% stayed on ARBs after 12 months. Only 57% stayed on ACE inhibitors. The reason? Fewer side effects. Patient reviews on Drugs.com give ARBs a 7.1/10 rating versus 5.8/10 for ACE inhibitors. Reddit threads are full of posts like: "Switched from lisinopril to valsartan - cough vanished in three days. Best decision I ever made."
Beta-Blockers: Not for Everyone - But Essential for Some
Beta-blockers like metoprolol, carvedilol, and bisoprolol work differently. Instead of relaxing blood vessels, they slow the heart. They reduce heart rate by 10-15 beats per minute and lower cardiac output. That’s why they’re not the first choice for general high blood pressure. Studies like the INVEST trial showed they’re worse than calcium channel blockers at preventing strokes.
But here’s where they shine: after a heart attack. The COMMIT trial found beta-blockers cut cardiovascular death by 23% in post-MI patients. That’s why they’re still first-line after a heart attack - even if the patient doesn’t have heart failure. The same goes for heart failure with reduced ejection fraction (HFrEF). Carvedilol cut all-cause mortality by 35% in the COPERNICUS trial. Atenolol? Not so much. It showed no mortality benefit in the LIFE trial. That’s why doctors now avoid atenolol for routine hypertension.
The downside? Fatigue. Up to 28% of people on beta-blockers feel exhausted. One user wrote: "Metoprolol made me so tired I couldn’t work. Switched to amlodipine - energy came back." Some beta-blockers are worse than others. Non-selective ones like propranolol can trigger asthma attacks. Even selective ones like metoprolol can raise triglycerides and lower HDL ("good" cholesterol) by 5-10%. But newer agents like nebivolol cause less fatigue - only 14% report it versus 28% with metoprolol.
What About Combining Them?
Many people need more than one drug. Combining an ACE inhibitor or ARB with a thiazide diuretic (like hydrochlorothiazide) is common and effective. Together, they can drop systolic pressure by 20-25 mmHg - more than either alone.
But there’s one dangerous combo to avoid: ACE inhibitor + ARB. The ONTARGET trial in 2008 proved this doubles the risk of kidney failure, high potassium, and low blood pressure. No benefit. Just harm. So if you’re on one, don’t add the other.
Now, a new option is emerging: sacubitril-valsartan (Entresto). It’s not just an ARB - it’s an ARB paired with a neprilysin inhibitor. The PARADIGM-HF trial showed it beat enalapril (an ACE inhibitor) in heart failure patients, reducing death by 20%. It’s now recommended as first-line for HFrEF by the European Heart Failure Association. But it carries a slightly higher risk of angioedema (0.5% vs 0.2%) - so it’s not for everyone.
Which One Should You Be On?
There’s no one-size-fits-all. Here’s how doctors decide:
- Diabetes + kidney disease → ACE inhibitor (best kidney protection)
- Post-heart attack → Beta-blocker (proven to save lives)
- Heart failure with reduced ejection fraction → Sacubitril-valsartan (if eligible), otherwise ACE inhibitor or ARB
- General high blood pressure with no other conditions → ARB (better tolerability) or ACE inhibitor (if cost is a factor)
- Side effects from ACE inhibitor → Switch to ARB - it’s almost always the fix
- Fatigue from beta-blocker → Try nebivolol or switch to calcium channel blocker
Start doses matter too. Most patients begin with lisinopril 10 mg, losartan 50 mg, or metoprolol succinate 25 mg. These are adjusted slowly. Don’t expect instant results - it takes weeks. And never stop these meds without talking to your doctor. Suddenly stopping beta-blockers can trigger a heart attack.

What’s Changing in 2026?
Guidelines keep evolving. The 2023 AHA guidelines now suggest ARBs over ACE inhibitors for new patients needing renin-angiotensin system blockade - unless they have post-MI or diabetic kidney disease. The PRECISION trial (due to finish in 2025) is studying whether ARBs protect brain health better than ACE inhibitors in older adults. Early data suggests ARBs may slow cognitive decline.
Market trends reflect this shift. ARBs are growing faster than ACE inhibitors. By 2028, they’re expected to lead the hypertension market. But ACE inhibitors won’t disappear. They’re still irreplaceable in heart attack recovery and diabetic kidney care.
And the future? Fixed-dose combos are coming. In 2023, the FDA approved a four-drug pill for hard-to-treat hypertension. It combines an ARB, two diuretics, and a calcium blocker. That’s the next frontier: fewer pills, better control, fewer side effects.
Can I switch from an ACE inhibitor to an ARB if I have a cough?
Yes - and it’s the most common solution. If you develop a persistent dry cough from an ACE inhibitor, switching to an ARB like losartan or valsartan usually eliminates the cough within days. Studies show 89% of patients who stop ACE inhibitors due to cough find relief with ARBs. There’s no drop in blood pressure control, and the risk of serious side effects like angioedema is much lower.
Why aren’t beta-blockers used as first-line for high blood pressure anymore?
Because they’re less effective at preventing strokes compared to other drugs like ARBs, ACE inhibitors, or calcium channel blockers. Trials like INVEST showed higher stroke rates with atenolol. They also tend to cause fatigue, weight gain, and worsen blood sugar and cholesterol levels. Today, beta-blockers are reserved for specific cases: after a heart attack, in heart failure, or if other drugs aren’t tolerated.
Is it safe to take an ARB and a beta-blocker together?
Yes - and it’s often recommended. Many patients with heart failure or high blood pressure plus other conditions (like diabetes or past heart attack) need multiple drugs. Combining an ARB with a beta-blocker like carvedilol or bisoprolol is standard practice. This combo reduces strain on the heart from two angles: relaxing blood vessels and slowing heart rate. It’s well-studied and proven to improve survival.
Do ARBs cause less fatigue than beta-blockers?
Yes. ARBs are generally energy-neutral. Most people don’t report fatigue from them. Beta-blockers, especially older ones like metoprolol, cause fatigue in up to 28% of users. If you’re tired on a beta-blocker, switching to an ARB might help - especially if your main issue is high blood pressure without heart failure. Always check with your doctor before switching.
What’s the most common reason people stop taking their blood pressure medication?
Side effects. For ACE inhibitors, it’s cough. For beta-blockers, it’s fatigue or dizziness. For ARBs, it’s rare - only about 15% report any side effects. That’s why adherence is highest with ARBs. One study found 63% of patients stayed on ARBs after a year, compared to just 57% on ACE inhibitors. If you’re struggling with side effects, talk to your doctor. There’s almost always a better option.
Final Thoughts
There’s no "best" antihypertensive. What works for your neighbor might not work for you. The goal isn’t just lowering numbers - it’s staying healthy, avoiding hospital visits, and living without side effects that ruin your day. ACE inhibitors save lives in heart attack and kidney disease. ARBs are easier to live with for most people with plain high blood pressure. Beta-blockers are lifesavers after a heart attack - but not for everyday use. The right choice depends on your history, your symptoms, and your goals. Don’t just take what’s prescribed - ask why. And if something feels off, speak up. There’s always a better fit.

Comments (14)
Lyle Whyatt
Man, I was on lisinopril for like a year and thought I was just getting old - coughing every night like I had a cold that never left. Then I switched to valsartan and it was like someone flipped a switch. No more 3 a.m. coughing fits. I could actually sleep. My wife said I stopped sounding like a dying seal. Seriously, if you’re on an ACE inhibitor and coughing, just switch. It’s not even a debate. ARBs are the quiet MVP of hypertension meds.
Also, side note: I went from 140/90 to 120/78 and didn’t gain weight or feel like a zombie. Beta-blockers? No thanks. I’ve seen too many people on metoprolol shuffle around like they’re dragging a coffin.
Just say no to fatigue. Say yes to feeling human again.
Random Guy
so like… ACE inhibitors make you cough like you’re in a horror movie and ARBs are the sequel where no one dies except your cough? yeah. i’m sold. also why does everyone on beta blockers look like they just lost a fight with a treadmill?
Brett Pouser
I’m a nurse in a rural clinic, and I’ve seen this play out a hundred times. Patient comes in, on lisinopril, can’t sleep, feels like they’re dying - but it’s just the damn cough. We switch to losartan, and boom. They’re back to playing with their grandkids, hiking, cooking dinner. No more ‘I think I’m getting pneumonia’ panic.
And honestly? The fatigue from beta-blockers is real. I had a 68-year-old patient who quit his job because he couldn’t stay awake past 3 p.m. Switched him to amlodipine and now he’s coaching Little League. That’s the kind of win we need more of.
Joshua Smith
Just curious - when you say ARBs are better tolerated, is that mostly because of the cough, or are there other side effects that are less common? I’ve heard people say they get dizzy or have weird taste sensations. Also, is there a difference between losartan and valsartan, or are they pretty much interchangeable?
Trying to understand the nuances so I can ask my doc better questions.
Jessica Klaar
My mom was on lisinopril for years. She didn’t even realize the cough was from the pill - thought it was allergies or dust. Then she switched to candesartan and said, ‘It’s like my lungs got a vacation.’ She’s 72 and now walks 4 miles every morning. No more wheezing at the grocery store.
I wish more doctors just said, ‘Try this instead’ instead of ‘Stick with it, it’ll get better.’ Sometimes the fix is simple. And it’s not just about numbers - it’s about being able to breathe.
PAUL MCQUEEN
Wow. So we’re just gonna ignore the fact that ARBs cost 3x more than lisinopril? And that the ‘better tolerability’ is mostly just avoiding a cough that’s not even dangerous? Meanwhile, beta-blockers save lives post-MI and are dirt cheap.
It’s like we’re treating hypertension like a lifestyle brand now. ‘Oh honey, your ARB has a 7.1/10 rating on Drugs.com - that’s better than his 5.8.’
Real talk: if you’re healthy, don’t need a drug. If you do, take the one that works. Not the one with the best Yelp reviews.
John Watts
You guys are talking about meds like they’re coffee flavors. Let me remind you - this isn’t about preference. This is about survival.
My dad had a heart attack at 61. They put him on metoprolol. He was tired, yes. But he’s alive. Three years later, no second event. No stroke. No hospital. That’s the power of beta-blockers. Don’t downplay it because someone got tired.
And if you’re on an ARB because you hate coughing? Good for you. But don’t act like it’s a ‘better’ drug overall. It’s just better for *you*. Context matters. Always.
Chima Ifeanyi
Let’s deconstruct this with some epidemiological rigor. The RENAAL trial’s 21% reduction in proteinuria is statistically significant, yes - but the absolute risk reduction? 0.7% over 3 years. Meanwhile, the NNT for ARB vs ACEI to prevent one cough-related discontinuation is 8.3. That’s a trade-off of marginal renal benefit for a massive adherence advantage.
Also, the 78% discontinuation rate for ACEI? That’s not a side effect - it’s a systemic failure of patient education. You don’t tell someone ‘you’ll get a cough’ - you say ‘you might get a dry tickle, here’s how to manage it.’
And sacubitril-valsartan? It’s not a ‘new option’ - it’s a $1,200/month luxury. The PARADIGM-HF trial excluded 92% of real-world hypertensives. Stop marketing this as a panacea.
Elan Ricarte
So let me get this straight - we’re telling people with high blood pressure to take a pill that makes them cough like they’re being strangled… but if they switch to a pill that costs 4x more and doesn’t make them sound like a broken foghorn, suddenly it’s ‘better’?
And beta-blockers? Oh no, they make you tired! But wait - they also prevent death! So… we’re prioritizing naptime over *living*?
Y’all are treating hypertension like a TikTok trend. ‘I’m on ARBs, my blood pressure is chill, my dog loves me more.’
Get real. Medicine isn’t a Spotify playlist. Some pills make you feel like crap - but they keep you from ending up in a body bag. That’s not ‘tolerability.’ That’s survival. And you’re not entitled to feel ‘energized’ while your arteries turn to concrete.
Angie Datuin
I’ve been on losartan for 3 years. Never had a cough. Never felt tired. Just… normal. I don’t even think about it anymore. That’s the goal, right? Not to feel amazing - just to feel okay.
My mom had a stroke because her BP wasn’t controlled. I don’t take this lightly. I just want to live long enough to see my niece graduate. And this pill helps me do that. No drama. No hype. Just… peace.
Camille Hall
One thing I’ve learned working in community health: adherence is everything. A perfect drug that no one takes does zero good. ARBs win here not because they’re ‘better’ - but because people *stay* on them. And that’s what saves lives in the long run.
It’s not about the science alone. It’s about real life. Someone who can’t sleep because of a cough isn’t going to refill their prescription. And then - boom - stroke. That’s not a side effect. That’s a failure of the system.
So yeah, ARBs aren’t perfect. But they’re the bridge that gets people to the other side.
Ritteka Goyal
India has 130 million hypertensives and 90% can't afford ARBs. We use lisinopril because it's 10 rupees a month. You think Americans are suffering? Try living in a village with no pharmacy and no doctor. We don't care about coughs - we care about not dying before 50.
Also, beta-blockers? We use them for everything - because they're cheap and work. Your ‘fatigue’ is a luxury. We don’t have the luxury of switching.
Stop acting like hypertension is a first-world problem. It’s not. And your ARB reviews? They’re not the standard. Survival is.
Tricia O'Sullivan
Thank you for this comprehensive and clinically nuanced overview. It is refreshing to encounter a discourse that eschews sensationalism in favour of evidence-based nuance. The distinction between pharmacodynamic efficacy and real-world tolerability is often conflated, yet remains paramount in chronic disease management. I concur with the assertion that ARBs represent a superior option for primary hypertension in the absence of compelling indications for ACE inhibition. The persistence data is particularly compelling, as it reflects patient-centred outcomes rather than purely clinical endpoints. I look forward to the PRECISION trial results with considerable interest.
Scott Conner
wait so if i switch from lisinopril to valsartan i stop coughing but do i still get the kidney protection? or is that only with ace inhibitors? just wanna make sure i’m not trading one problem for another. also, is there a generic version of that new combo pill? lol