What really causes type 2 diabetes?
You might think type 2 diabetes is just about eating too much sugar. But that’s not the full story. The real problem starts long before your blood sugar climbs into the danger zone. It begins with something called insulin resistance-a quiet, invisible breakdown in how your body uses insulin. This isn’t a sudden failure. It’s a slow, years-long process where your cells stop listening to insulin, the hormone that tells them to soak up glucose from your blood. And when that happens, your pancreas works harder and harder to keep up-until it can’t anymore.
That’s when type 2 diabetes kicks in. But insulin resistance doesn’t show up alone. It’s the engine behind a cluster of conditions doctors now call metabolic dysfunction syndrome (MDS)-a term replacing the older label ‘metabolic syndrome’ because it better reflects what’s actually going wrong inside your body. This isn’t just about weight or high blood pressure. It’s about your entire metabolism going off track.
How insulin resistance starts-and why it’s so hard to spot
Insulin resistance doesn’t come with a warning sign. No rash. No fever. Just fatigue. A slow weight gain around the middle. Difficulty losing weight, no matter how hard you try. And constant hunger-even after eating.
Here’s what’s happening at the cellular level: when you eat too many refined carbs and sugars over time, your body floods your bloodstream with glucose. In response, your pancreas pumps out more insulin. Fat cells, liver cells, and muscle cells start getting overloaded. They stop responding properly to insulin’s signal. Glucose stays in your blood. Your pancreas responds by making even more insulin. This cycle goes on for years. By the time your fasting blood sugar hits 100 mg/dL, you’re already deep into insulin resistance.
Research from the University of Texas shows that 80-90% of people with type 2 diabetes had insulin resistance years before their diagnosis. And it’s not just about being overweight. About 30-40% of people with normal weight still develop insulin resistance, especially if they carry fat deep inside their abdomen or liver. That’s why two people can look the same on the outside but have completely different metabolic health.
Metabolic syndrome: More than just a list of numbers
Doctors diagnose metabolic syndrome when you have at least three of these five things:
- Waist size over 94 cm for men (or 80 cm for women)-especially if you’re of South Asian, Chinese, or Japanese descent
- Triglycerides above 150 mg/dL
- HDL (good) cholesterol below 40 mg/dL for men or 50 mg/dL for women
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar of 100 mg/dL or higher
But these aren’t just random numbers. They’re all connected by one thing: insulin resistance. High triglycerides? Your liver is dumping fat into your blood because it can’t process glucose properly. Low HDL? Insulin messes with how your body handles cholesterol. High blood pressure? Excess insulin makes your kidneys hold onto sodium and water. And that belly fat? It’s not just storage-it’s active tissue releasing inflammatory chemicals that make insulin resistance worse.
The scary part? Having metabolic syndrome doesn’t just raise your risk of diabetes. It triples your chance of having a heart attack or stroke. The Mayo Clinic found that people with this combination of factors have a 200-300% higher risk of cardiovascular disease than those without any of them.
Prediabetes vs. type 2 diabetes: Where does the line get crossed?
Prediabetes means your blood sugar is higher than normal-but not high enough to be called diabetes yet. That’s usually a fasting glucose between 100 and 125 mg/dL. At this stage, your pancreas is still working overtime. Beta cells are producing plenty of insulin, but your body just won’t use it.
But over time, those beta cells get worn out. Studies from Joslin Diabetes Center show they decline by 4-5% per year in people with insulin resistance. Once they can’t keep up, your blood sugar spikes past 126 mg/dL fasting-or 200 mg/dL after eating. That’s when you cross into type 2 diabetes.
Here’s the key difference: prediabetes is reversible. Type 2 diabetes is manageable-but rarely cured. That’s why catching insulin resistance early is everything.
Who’s most at risk-and why
It’s not just about being overweight. While obesity is a major factor, genetics play a huge role. People of South Asian, African, or Indigenous descent often develop insulin resistance at lower body weights. That’s why waist size matters more than BMI in these groups.
And it’s not just lifestyle. A growing number of lean individuals-especially those with fatty liver disease-are developing type 2 diabetes. Research from Oxford University shows that in some cases, beta cell dysfunction is the main driver, not insulin resistance. This is especially true in younger, leaner patients with a strong family history.
Nonalcoholic fatty liver disease (NAFLD) is a huge red flag. If you have fat in your liver, your risk of type 2 diabetes more than doubles. And if you have the more serious form, NASH, your risk jumps even higher. That’s because your liver is the first organ to become insulin resistant-and it’s the one that controls your blood sugar levels most tightly.
What actually works to reverse insulin resistance
Medication can help-but lifestyle changes are the only thing that can truly reverse the process.
The Diabetes Prevention Program (DPP) proved this decades ago. People with prediabetes who lost just 7% of their body weight and walked 150 minutes a week cut their risk of developing type 2 diabetes by 58%. That’s more effective than metformin, the most common diabetes drug.
Here’s what works:
- Weight loss: Even 5-7% of your body weight improves insulin sensitivity dramatically. For someone weighing 90 kg, that’s just 4.5-6 kg.
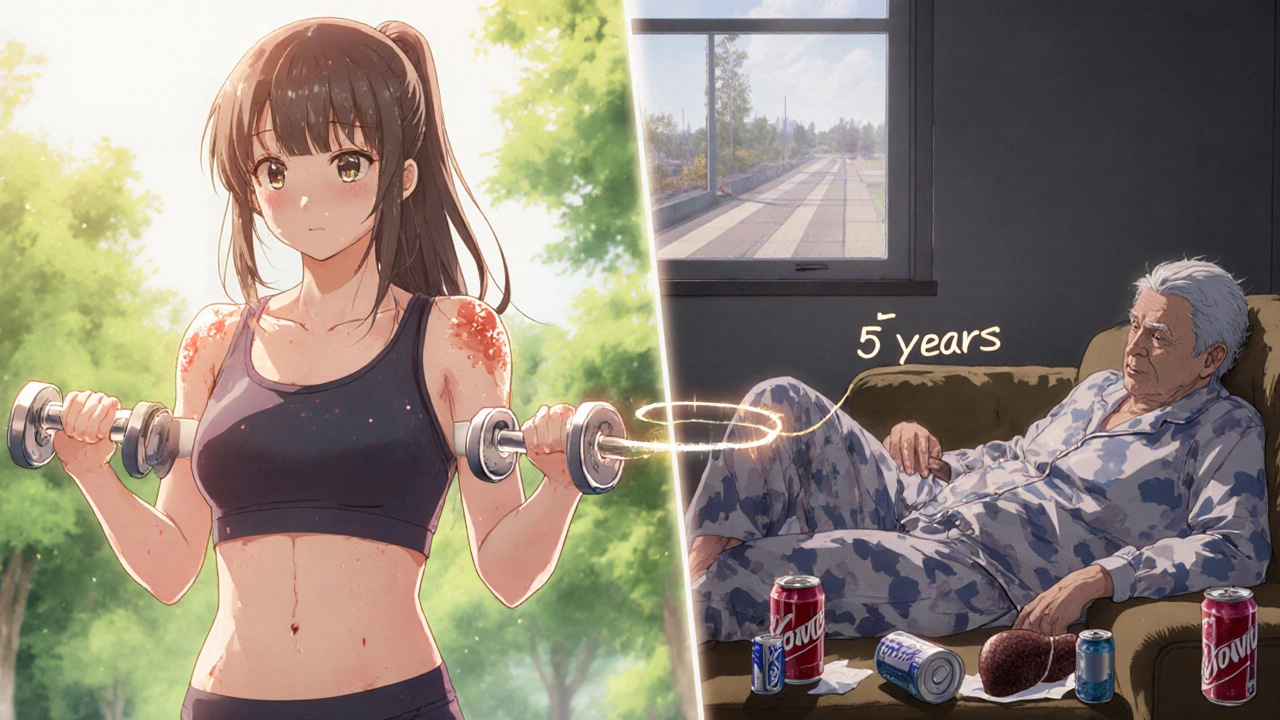
- Resistance training: Muscle is the body’s main glucose sink. Lifting weights or doing bodyweight exercises 2-3 times a week improves insulin sensitivity better than cardio alone.
- Reducing refined carbs: White bread, sugary drinks, pastries-they spike insulin and keep it high. Swap them for whole grains, legumes, vegetables, and healthy fats.
- Sleep and stress: Chronic stress raises cortisol, which increases blood sugar. Poor sleep reduces insulin sensitivity. Both are silent drivers of metabolic dysfunction.
The Look AHEAD trial showed that people who lost 10% of their weight in the first year had a 51% chance of reversing their diabetes. Twelve percent were still in remission eight years later. That’s not a miracle. That’s science.

What’s new in treatment-and what’s overhyped
New drugs like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro) are changing the game. They don’t just lower blood sugar. They help you lose weight, reduce liver fat, and lower blood pressure. In the STEP trials, people lost nearly 15% of their body weight on average. In the SELECT trial, 66% of patients with type 2 diabetes went into remission.
But these aren’t magic pills. They work best when combined with lifestyle changes. And they’re expensive. Most people can’t access them long-term without insurance.
Stem cell therapies are also emerging. Vertex Pharmaceuticals’ VX-880 trial showed 71% of patients stopped needing insulin after one year. But this is still experimental. It’s not available outside clinical trials.
Don’t fall for quick fixes. Detox teas, miracle supplements, or extreme keto diets won’t fix insulin resistance. They might help short-term-but without lasting lifestyle change, the problem comes back.
The bottom line: Your body is trying to tell you something
Type 2 diabetes isn’t a punishment for eating too much cake. It’s the result of years of metabolic stress. Insulin resistance is the hidden thread tying together obesity, fatty liver, high blood pressure, and heart disease. And it’s happening to millions of people who think they’re fine because they’re not ‘obese’ or ‘diabetic’ yet.
If you have a big waistline, high triglycerides, low HDL, or borderline blood sugar-don’t wait. Get tested. Ask for an HbA1c, fasting insulin, and liver ultrasound. Don’t accept ‘it’s just aging’ or ‘you’re fine for now.’
Reversing insulin resistance isn’t about perfection. It’s about consistency. One less sugary drink a day. A 20-minute walk after dinner. Getting seven hours of sleep. These small things add up. And they’re the only things that can truly change your trajectory.
The future of metabolic health isn’t in pills. It’s in awareness. In action. In choosing to listen to your body before it breaks down.
Can you reverse insulin resistance without medication?
Yes. Studies like the Diabetes Prevention Program show that losing 5-7% of your body weight and getting 150 minutes of moderate exercise per week can reverse insulin resistance in most people. Lifestyle changes are more effective than metformin at preventing type 2 diabetes. Medication can help, but it doesn’t fix the root cause.
Is metabolic syndrome the same as type 2 diabetes?
No. Metabolic syndrome is a cluster of risk factors-including insulin resistance, high blood pressure, abnormal cholesterol, and belly fat-that make type 2 diabetes much more likely. You can have metabolic syndrome without being diabetic. But if you have it, your risk of developing type 2 diabetes is 5-6 times higher than someone without it.
Why do some thin people get type 2 diabetes?
Thin people can still have visceral fat-fat stored deep inside the abdomen and liver-that causes insulin resistance. Genetics also play a role. People of South Asian, African, or Indigenous descent often develop metabolic problems at lower body weights. Beta cell dysfunction, not just insulin resistance, can be the main driver in these cases.
Does fasting help with insulin resistance?
Intermittent fasting can help by lowering insulin levels and giving your cells a break from constant glucose exposure. Studies show it improves insulin sensitivity, especially when combined with reduced carb intake. But it’s not a magic solution. If you return to a high-sugar diet afterward, the benefits disappear. Consistency matters more than the timing of meals.
How often should I get tested if I have metabolic syndrome?
Check your HbA1c every 3-6 months if you’re prediabetic or have metabolic syndrome. Monitor your blood pressure and cholesterol at least once a year. If you’re making lifestyle changes, retest fasting insulin and liver enzymes annually to track progress. Don’t wait for symptoms-by then, it’s often too late.
Can exercise alone fix insulin resistance?
Exercise is powerful-but not enough on its own. Combining strength training and cardio improves insulin sensitivity significantly. But if you’re still eating a high-sugar, high-refined-carb diet, your body will keep producing excess insulin. Diet and movement together are the most effective combo. Muscle burns glucose, but only if you give it the right fuel.
Are GLP-1 drugs like Ozempic a cure for type 2 diabetes?
No. They’re powerful tools that help you lose weight and lower blood sugar, and many people go into remission while using them. But if you stop the medication and return to old habits, the diabetes usually comes back. They treat the symptoms, not the root cause. Long-term remission still requires lasting lifestyle changes.
What to do next
If you’re concerned about insulin resistance or metabolic syndrome, start with three simple steps:
- Get your HbA1c, fasting glucose, and triglycerides tested. Ask for a waist measurement and liver ultrasound if you’re overweight or have a family history.
- Reduce sugar and refined carbs. Swap white bread for sourdough, soda for sparkling water, and snacks for nuts or fruit.
- Move daily. Walk 30 minutes after meals. Add two strength sessions a week. You don’t need a gym-bodyweight squats, push-ups, and lunges work.
Don’t wait for a diagnosis. The earlier you act, the more control you have. Your body doesn’t need a miracle. It just needs you to stop fighting it-and start working with it.


Comments (13)
Daisy L
This is why America’s health is collapsing. Sugar is poison. Big Pharma and the USDA are in bed together. We’re being fed lies while our kids get diabetic at 12. I’m done pretending this is about ‘choice’.
STOP EATING WHITE STUFF. START MOVING. OR GET LEFT BEHIND.
Anne Nylander
Yessss!! I was prediabetic last year and just started walking after dinner and cutting out soda. Lost 8 lbs in 6 weeks and my doctor was SHOCKED. You don’t need to be perfect, just consistent!! 🙌💪 You got this!
Noah Fitzsimmons
Oh wow, another ‘lifestyle change’ miracle cure. Tell me, genius, why did my uncle lose 30 lbs on keto and still end up on insulin? Maybe the problem isn’t carbs-it’s your damn beta cells failing. Science isn’t a TikTok trend.
Sheldon Bazinga
So basically, if you’re not a white, middle-class American with access to organic kale and a Peloton, you’re screwed? Cool. Thanks for the elitist lecture on how poor people cause their own diabetes. 🙄
Cooper Long
The data is unequivocal. Insulin resistance precedes hyperglycemia by years. The metabolic syndrome construct remains clinically useful despite semantic objections. Lifestyle intervention remains the only intervention with sustained efficacy in peer-reviewed longitudinal studies.
Leo Tamisch
We’ve reduced the human body to a biochemical algorithm. Insulin resistance? More like a spiritual disconnection from nature. We’ve forgotten how to eat, how to move, how to breathe. The body whispers. We scream into the void with metformin and Ozempic. 🌿💔
Kartik Singhal
In India, we’ve seen this for decades. Thin people, high belly fat, diabetes at 35. It’s not about weight. It’s about rice, ghee, and stress. The system is rigged. But guess what? My aunty reversed it with millet roti and 45 min walks. No pills. Just patience. 🙏
Chris Vere
The real tragedy is how few people know this before its too late. I’m 38 and just got diagnosed with prediabetes. I thought I was fine because I wasn’t fat. Turns out my liver was screaming and I didn’t even hear it. This post saved me from denial. Thank you.
Mark Kahn
You don’t need to overhaul your life tomorrow. Start with one thing. Swap your morning donut for an egg. Walk 10 minutes after lunch. Drink water instead of juice. Small wins add up. I’m proud of you for reading this. Now go take that first step. 🌞
Sandi Moon
Let’s not ignore the elephant in the room: glyphosate. The USDA approved it as ‘safe’ while insulin resistance rates skyrocketed. Coincidence? Or corporate science? The liver doesn’t lie. The data doesn’t lie. The government? That’s another story. 🕵️♂️
Pravin Manani
The key insight here is that insulin resistance is a systemic failure, not a personal failing. The body adapts to chronic glucose overload. It’s not weakness-it’s biology. That’s why one-size-fits-all advice fails. We need personalized metabolic profiling. Not moralizing.
Logan Romine
So Ozempic works… but only if you’re rich? And if you’re poor, you just get told to ‘eat less sugar’? Cool. So the cure for a systemic crisis is… individual discipline? Thanks for the classist pep talk, doc. 😌
Franck Emma
I lost my dad to this. He was thin. He ate ‘healthy.’ He walked every day. He was still gone by 58. No one told him his liver was rotting. This isn’t prevention. It’s a silent genocide. And they’re selling pills to make it feel like we’re doing something.