Rivastigmine: a clear guide for patients and caregivers
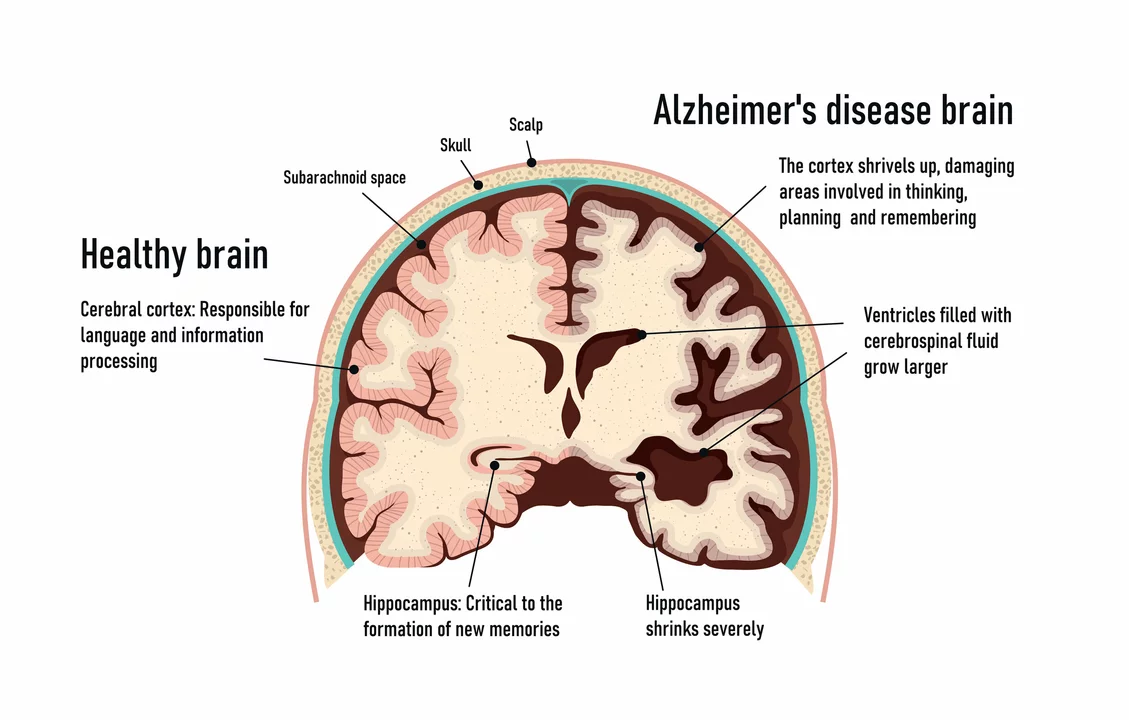
Rivastigmine is a medication that can help thinking and memory in people with mild to moderate Alzheimer's disease and dementia linked to Parkinson's disease. It is not a cure, but many patients notice slower memory loss or better daily functioning for months after starting treatment. Knowing what to expect and how to manage side effects makes the difference.
How rivastigmine works and who it's for
Rivastigmine boosts acetylcholine, a brain chemical that helps neurons communicate. Doctors use it when memory, attention, or daily tasks start to decline. The drug comes as oral capsules or a once-daily transdermal patch. The patch is helpful for people who have trouble swallowing or who can't tolerate stomach upset from the pills.
Practical tips: dosing, side effects, and caregiver advice
Typical oral dosing starts low—often 1.5 mg twice a day—then rises every two weeks if tolerated up to 6 mg twice daily. Patches are labeled by the amount released in 24 hours: 4.6 mg, 9.5 mg, and 13.3 mg. Doctors raise doses slowly to reduce nausea and vomiting, which are the most common early problems.
Common side effects include nausea, vomiting, diarrhea, loss of appetite, weight loss, and increased sweating. These usually occur during the first few weeks or when the dose increases and often improve over time. Serious but rarer problems are slow heart rate, fainting, stomach bleeding, and breathing trouble in people with reactive airways disease.
Share a full medicine list with your prescriber. Anticholinergic drugs can counteract rivastigmine. Medicines that lower heart rate, like some beta-blockers, increase the risk of bradycardia. NSAIDs can raise the chance of stomach bleeding, especially if someone is already prone to ulcers. Also tell the doctor about past fainting, seizures, or breathing problems before starting.
Clinicians usually monitor weight, heart rate, and blood pressure after starting or changing doses. If stomach symptoms are severe, your doctor may slow the increase or switch from pills to the patch. If serious side effects like fainting or fast worsening of breathing appear, stop the drug and seek care.
Caregivers should track daily abilities—dressing, eating, sleep, falls—and note any side effects. For the patch: apply to clean, dry, hairless skin on the upper back or chest; rotate sites and press firmly for 30 seconds. Replace it every 24 hours. If a patch falls off, replace it right away. For pills, give with food to lower nausea risk.
Benefits are modest. Some people get clearer thinking or easier daily tasks for a few months; others see no change. Talk with your doctor about realistic goals and timelines. Rivastigmine is sold as brand Exelon and as generics, which may cost less—ask a pharmacist about options and insurance coverage.
If cost or access is an issue, ask about samples, assistance programs, or telemedicine options today.
Questions about rivastigmine—how fast it works, side effects, or stopping the treatment—are worth discussing with the prescriber. Slow dose changes, good notes on behavior and side effects, and open communication with the care team make this treatment easier and safer.
The Role of Nutrition and Rivastigmine in Alzheimer's Disease Management
In my latest blog post, I explored the crucial role of nutrition and Rivastigmine in managing Alzheimer's disease. I discussed how a balanced diet rich in antioxidants, omega-3 fatty acids, and other essential nutrients can potentially slow down cognitive decline. Additionally, I delved into the benefits of Rivastigmine, a medication proven to alleviate some Alzheimer's symptoms by enhancing memory and cognitive function. Through this post, I aim to raise awareness about the importance of a comprehensive approach to Alzheimer's management and encourage further research in this field. So, if you or a loved one are affected by this condition, I highly recommend giving it a read to learn more about these valuable strategies.
View More