Hypophosphatemia: Low Phosphate Symptoms, Causes, and Fixes
Hypophosphatemia means your blood phosphate is too low. Phosphate helps build bones, make energy, and keep muscles and nerves working. When levels fall you might feel weak, tired, or confused. Mild drops often cause no symptoms, but severe hypophosphatemia can cause muscle breakdown, breathing trouble, or heart rhythm changes. Below you'll find clear signs, common causes, simple tests, and practical treatments.
How do you know you have it? Doctors check phosphate with a blood test. Normal adult phosphate sits roughly between 2.5 and 4.5 mg/dL, though labs vary. If a routine panel shows low phosphate your provider will look for what caused it and how fast it fell. Rapid drops need faster treatment than slow, chronic low levels.
Common causes to watch
Several things can lower phosphate. Poor nutrition or alcohol use cuts intake and absorption. Long-term antacid or phosphate binder use reduces uptake. Certain medicines like diuretics or intravenous antacids after surgery can shift phosphate out of blood. Hormone problems, especially high parathyroid hormone, push phosphate into urine. Refeeding after starvation and sudden recovery from diabetic ketoacidosis can cause a sharp drop too.
Symptoms and when to act
Early signs are vague: fatigue, muscle weakness, sore bones, slow reflexes, or irritability. If hypophosphatemia is moderate to severe you may notice stiff limbs, trouble breathing, chest pain, or numbness. Confusion, seizures, or irregular heartbeat are medical emergencies. Call your doctor if you have weakness that affects daily tasks, shortness of breath, or new chest discomfort.
Treatment depends on cause and severity. For mild cases improving diet and reducing offending drugs may be enough. Foods high in phosphate include dairy, nuts, seeds, whole grains, and meat. Oral phosphate supplements are common when diet alone won't correct levels. For severe or fast drops doctors use intravenous phosphate in the hospital while monitoring calcium and kidney function closely.
Prevention focuses on balance. If you have chronic conditions like alcoholism, malabsorption, or take medications that affect phosphate, ask your provider about regular blood checks. When starting aggressive nutrition after starvation, or treating diabetic ketoacidosis, medical teams should watch phosphate and replace it proactively.
Testing and follow up are simple: repeat blood phosphate and kidney tests until levels stabilize. If an underlying disease like hyperparathyroidism or vitamin D deficiency is found, treating that problem prevents recurrences. Most people respond well to targeted treatment and regain strength over days to weeks.
If you suspect severe hypophosphatemia or have worrying symptoms, seek urgent care. For mild concerns, make an appointment, bring a list of medications and supplements, and ask about a phosphate blood test. Small steps—like adjusting meds or adding phosphate-rich foods—often fix the problem without drama.
Don't take phosphate tablets without advice. Too much phosphate can upset calcium, cause deposits in soft tissues, or harm kidneys. People with kidney disease need a different plan. If your doctor prescribes oral phosphate, follow the dose and report nausea, diarrhea, or muscle cramps. Keep a simple log of symptoms during treatment. Daily.
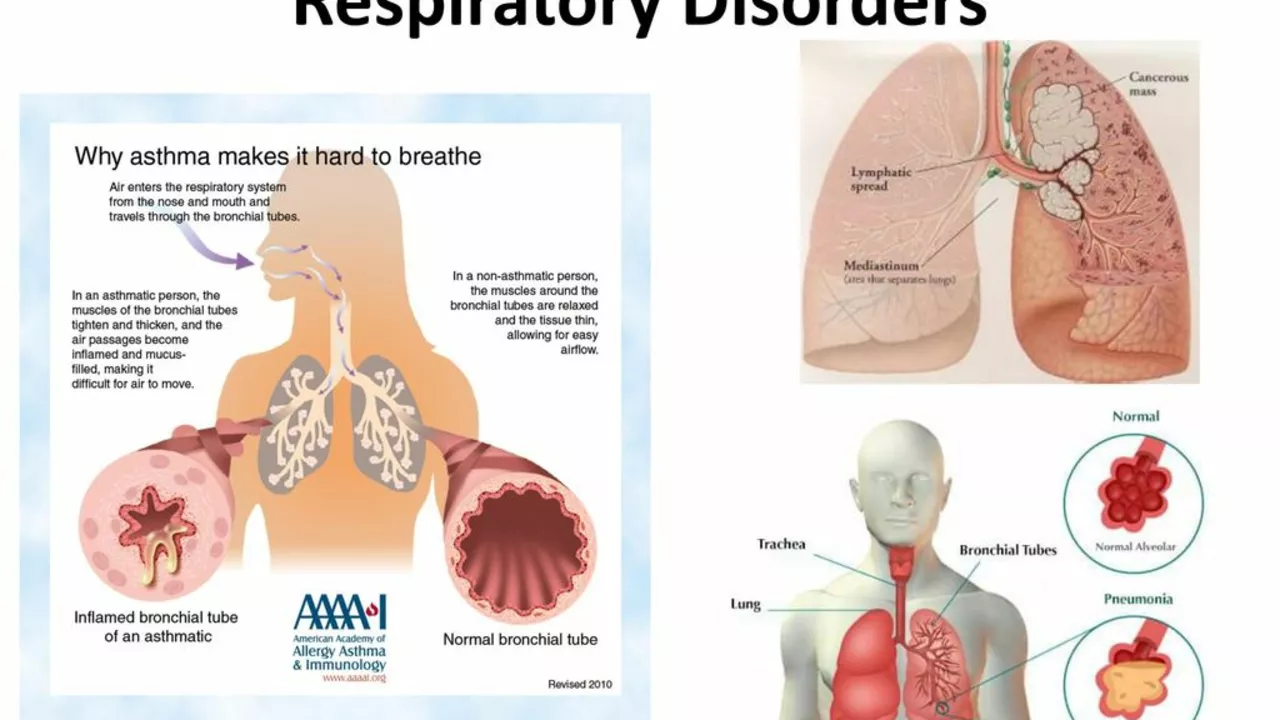
Hypophosphatemia and Respiratory Issues: What You Need to Know
In my recent blog post, I explored the connection between hypophosphatemia and respiratory issues. Hypophosphatemia is a condition marked by low phosphate levels in the blood, which can cause various health problems, including respiratory distress. It's essential to know that severe hypophosphatemia can weaken our respiratory muscles leading to difficulty in breathing. We also discussed how proper diagnosis and treatment can effectively manage these conditions. It's a vital read for anyone looking to broaden their understanding of the link between our respiratory health and our body's mineral balance.
View More