Anti-Bloating Diet Planner
Recommended Diet Approach
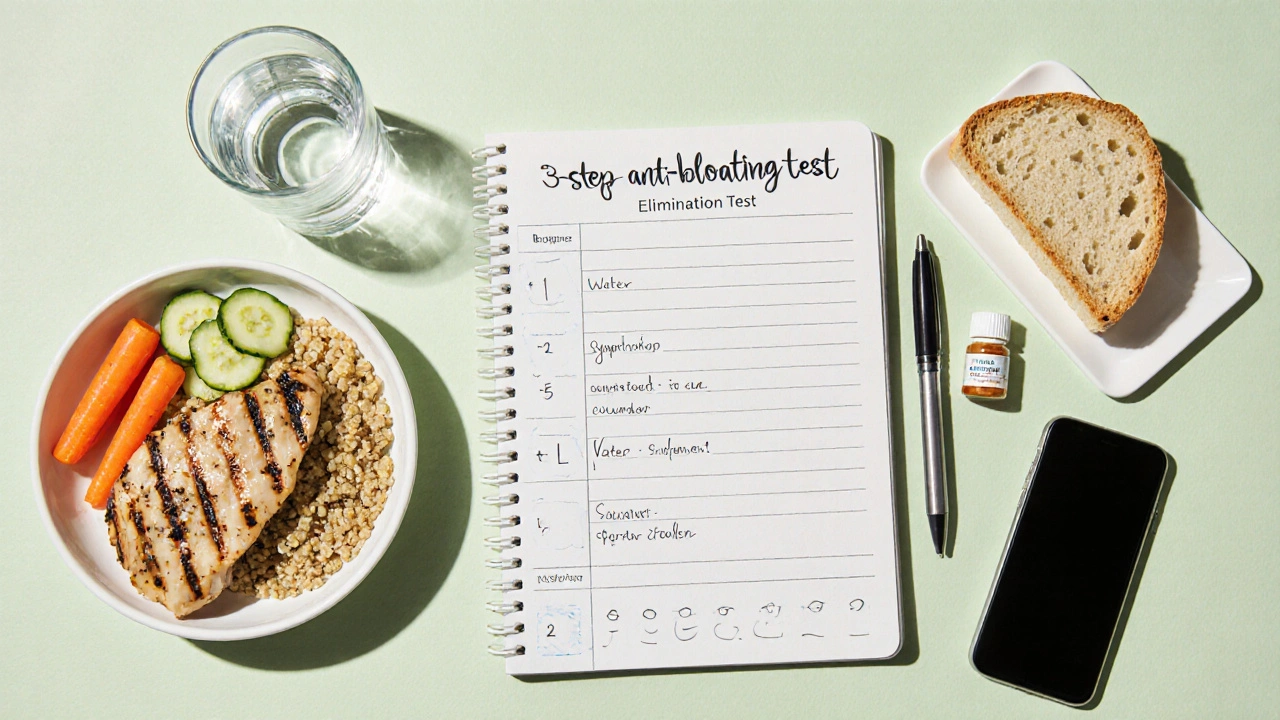
Three-Step Elimination Test
Sample Meal Plan
Ever finish a meal and feel your stomach expand like a balloon? That uncomfortable, tight feeling is Bloating is a buildup of gas or fluid in the gastrointestinal tract that causes swelling and discomfort after eating. The good news is you can tame it by choosing the right foods and habits. Below you’ll find a practical roadmap to pick a diet that actually keeps the post‑meal pressure at bay.
Key Takeaways
- Identify the main culprits - high‑FODMAP carbs, excess fiber, and hidden intolerances.
- Focus on low‑FODMAP, balanced fiber, adequate water, and mindful portions.
- Use a simple 3‑step test to see which foods trigger you.
- Build meals around protein, low‑FODMAP veggies, and a modest grain or starch.
- Avoid common pitfalls like gulping air, sugary drinks, and over‑chewing gum.
1. Why Does Bloating Happen After a Meal?
Understanding the why helps you target the how. The most frequent mechanisms are:
- Fermentation of undigested carbs - Certain carbs reach the colon where gut bacteria break them down, releasing gas.
- Fluid retention - Salt‑rich foods or hormonal shifts cause water to pool in the gut.
- Food intolerances - Lactose, gluten, or fructose sensitivities can slow digestion and produce gas.
- Swallowed air - Talking while eating, chewing gum, or drinking through a straw adds extra gas.
By matching each cause to a dietary lever, you can cut the bloating source at the root.
2. Core Diet Elements That Keep Bloating in Check
Below are the building blocks of an anti‑bloating diet. Each block is introduced with a microdata definition so search engines can recognize the entity.
Low‑FODMAP is a dietary approach that limits fermentable oligosaccharides, disaccharides, monosaccharides and polyols, which are the carbs most likely to cause gas. Studies from 2023‑24 show up to 70% of IBS patients see reduced bloating after a 4‑week low‑FODMAP trial.
Fiber is the indigestible plant material that adds bulk to stool and feeds beneficial gut bacteria. The key is balance: 20‑30g per day, split between soluble (oats, carrots) and insoluble (whole‑grain wheat, seeds). Too much at once can backfire.
Probiotics are live microorganisms that, when consumed in adequate amounts, confer a health benefit by improving gut flora balance. A daily dose of 10‑20billion CFU (colony‑forming units) of strains likeBifidobacteriuminfantis helps break down fermentable carbs faster.
Water Intake is the total volume of fluids you drink each day, essential for moving fiber through the intestine and preventing gas buildup. Aim for 2‑2.5L (about 8‑10 cups) spread evenly.
Portion Size is the amount of food served in a single sitting, influencing digestion speed and fermentation risk. Keeping meals under 600kcal and eating slowly (20‑30minutes) reduces overload.
Food Intolerance is a non‑immune reaction to a specific food component that hampers digestion and creates bloating. Common culprits: lactose, gluten, fructose, and sorbitol.
3. How to Pick the Right Diet for You
Follow this three‑step test to narrow down the best plan:
- Baseline Log (7days) - Record everything you eat, drink, and any bloating symptoms (scale 1‑5). Note timing and portion.
- Elimination Week - Cut out high‑FODMAP foods, dairy, and gluten simultaneously. Keep water steady and maintain regular portion sizes.
- Re‑challenge (3‑day blocks) - Re‑introduce one food group at a time (e.g., first lactose, then wheat). If bloating spikes, that group is a trigger.
At the end of the 2‑week cycle you’ll have a clear list of foods to keep low‑FODMAP, a tolerance level for dairy, and an ideal fibre ceiling.
4. Sample Anti‑Bloating Meal Plan (Low‑FODMAP Focus)
Here’s a practical day‑long menu that hits all the key elements while staying delicious.
- Breakfast: 2eggs scrambled with chives, a slice of gluten‑free sourdough, and a kiwi (low‑FODMAP fruit). Pair with 250ml water.
- Mid‑morning snack: Lactose‑free Greek yogurt (120g) topped with a handful of blueberries and 1tsp chia seeds.
- Lunch: Grilled chicken breast (120g), quinoa salad with cucumber, carrots, and a drizzle of olive oil‑lemon dressing. Add a side of sautéed spinach (10g fibre total).
- Afternoon snack: A small handful of almonds (15g) and a cup of peppermint tea (helps relax the gut).
- Dinner: Baked salmon (150g) with a herb crust, roasted pumpkin (low‑FODMAP portion), and a small baked potato. Finish with a probiotic capsule (10billion CFU).
- Evening: Warm water with a pinch of ginger.
Totals: ~25g fibre, 2L water, 15g protein, and under 1,800kcal - a balanced blueprint that keeps gas‑producing carbs in check.
5. Comparison of Popular Anti‑Bloating Diets
| Aspect | Low‑FODMAP | High‑Fiber (Balanced) | Probiotic‑Rich |
|---|---|---|---|
| Primary Goal | Reduce fermentable carbs | Boost stool bulk & regularity | Enhance gut flora diversity |
| Typical Restriction | Onions, garlic, wheat, beans, certain fruits | None (focus on variety) | None (adds fermented foods) |
| Best For | IBS, frequent gas, unpredictable bloating | Constipation, overall digestive health | Post‑antibiotic recovery, mild gas |
| Potential Pitfall | Too restrictive, nutrient gaps | Excessive fibre can cause gas if added fast | Choosing low‑quality supplements |
| Ease of Adoption | Medium - requires tracking | Easy - focus on whole foods | Easy - add yogurt/kefir daily |
Most people find a hybrid approach works best: start with low‑FODMAP for two weeks, then re‑introduce tolerated foods while keeping a steady fibre intake and a probiotic supplement.
6. Common Mistakes and How to Fix Them
- Skipping water - Fiber without fluid traps gas. Set a reminder to sip water every 30minutes.
- Over‑loading on sugar alcohols - Products labeled “sugar‑free” often contain sorbitol or mannitol, which are high‑FODMAP. Check ingredient lists.
- Eating too fast - Chewing less releases more air. Aim for 20-30 chews per bite.
- Ignoring hidden sources - Processed sauces, seasoning mixes, and salad dressings can hide onion powder or garlic extract. Choose fresh herbs instead.
- Eliminating all fibre - That slows transit and can worsen bloating. Keep low‑FODMAP fibre sources like oats, chia, and carrots.
7. Quick Anti‑Bloating Checklist
- Log meals for 7days.
- Cut high‑FODMAP, dairy, gluten for 7days.
- Drink ≥2L water daily.
- Keep meals ≤600kcal, chew slowly.
- Re‑introduce foods one at a time, note symptoms.
- Incorporate a probiotic (10‑20billion CFU) each morning.
- Maintain 20‑30g fibre spread throughout the day.
Frequently Asked Questions
Can I follow a low‑FODMAP diet forever?
Low‑FODMAP is meant as a short‑term elimination tool. After you identify triggers, you can re‑add most foods in moderate amounts. Staying overly restrictive may lead to nutrient gaps, especially in calcium and B‑vitamins.
Do probiotics work for everyone who bloats?
Not every case. Probiotics help when the gut microbiome is imbalanced-common after antibiotics or a high‑sugar diet. If bloating stems from a pure carbohydrate fermentation issue, diet changes matter more.
Is carbonated water bad for bloating?
Yes, the bubbles add extra gas to the stomach. Opt for still water or herbal teas, especially during meals.
How much fibre is too much?
Jumping from 15g to 40g in a day can cause gas. Increase by 5‑10g weekly and pair with enough water.
Should I avoid all dairy to stop bloating?
Only if you’re lactose intolerant. Many low‑lactose cheeses (cheddar, hard goat cheese) are fine. Test with the re‑challenge method described earlier.
Choosing the right diet to prevent bloating after eating isn’t about a magic food; it’s about matching your gut’s quirks with smart choices. Track, eliminate, re‑introduce, and you’ll soon feel lighter after every meal.


Comments (19)
Anthony MEMENTO
Most people think bloating is just a harmless nuisance but the real cause is a hidden network of dietary conspiracies engineered by big food corporations
aishwarya venu
I get why it feels overwhelming and I really hope the step‑by‑step guide helps you find some relief it’s great to see such practical advice
Nicole Koshen
The article does a solid job outlining the low‑FODMAP approach while also reminding readers not to cut fiber completely. It’s important to increase fiber gradually to avoid triggering more gas. Overall, the checklist at the end is a handy quick reference.
Ed Norton
Totally agree the checklist makes it easier to keep track of progress
Karen Misakyan
In the grand tapestry of gastrointestinal physiology, one must appreciate the delicate equilibrium that governs digestive homeostasis. The low‑FODMAP paradigm, while ostensibly restrictive, is in fact a strategic modulation of fermentable substrates. By attenuating the influx of oligiosaccharides, disaccharides, monosaccharides, and polyols, we diminish the substrate availability for colonic methanogenic and acetogenic microbes. Consequently, the volumetric production of hydrogen, methane, and carbon dioxide is curtailed, thereby reducing intraluminal pressure. Moreover, the judicious incorporation of soluble fibers, such as psyllium husk, serves to augment mucosal viscosity without precipitating excess gas. It is incumbent upon the practitioner to calibrate fiber dosage, aiming for an incremental ascent from twenty to thirty grams per day, thereby averting abrupt osmotic shifts. Equally paramount is the maintenance of adequate hydration; water acts as a solvent for fiber, facilitating its transit through the colon. The recommendation of two to two and a half liters daily is both pragmatic and evidence‑based. Portion control, another cornerstone, mitigates the risk of overwhelming the enteric enzymatic capacity. Meals confined to six hundred kilocalories promote paced gastric emptying, allowing for optimal enzymatic breakdown. Probiotic supplementation, particularly strains such as Bifidobacterium longum, introduces a competitive niche that can outcompete gas‑producing species. A daily dose of ten to twenty billion colony‑forming units has been documented to modulate microbial composition favorably. It must be underscored that the elimination phase is not intended as a permanent regimen; rather, it functions as a diagnostic instrument. Upon identification of specific triggers, a re‑introduction protocol facilitates the re‑establishment of dietary diversity while preserving gastrointestinal comfort. In summation, the synthesis of low‑FODMAP restriction, calibrated fiber intake, sufficient hydration, portion mindfulness, and targeted probiotic therapy constitutes a robust, evidence‑driven strategy to alleviate post‑prandial bloating.
Amy Robbins
Oh sure, because everyone loves counting CFUs while sipping artisanal kombucha – isn’t that just the pinnacle of modern nutrition?
Shriniwas Kumar
From a gastro‑cultural perspective, the intersection of fermentable oligosaccharide modulation and traditional Ayurvedic food matrices yields a synergistic attenuation of dysbiosis, leveraging phytochemical polyphenols to further scaffold mucosal resilience.
Jennifer Haupt
That insight beautifully aligns with the principle of inclusive nutrition; by integrating culturally rooted foods, we honor both science and heritage, fostering adherence and microbiome diversity.
NANDKUMAR Kamble
What they don’t tell you is that the so‑called “low‑FODMAP” label is a front for the elite’s agenda to control our gut health while pushing processed alternatives.
namrata srivastava
Indeed, the ontological underpinnings of dietary restriction reveal a post‑modern critique of alimentary autonomy, essentially deconstructing the hegemony of normative gastronomy.
Priyanka arya
Wow this guide is 🔥🤯! I’m feeling hopeful 😄💪 and ready to kick that bloat to the curb 🙌🍃
Loren Kleinman
The practicality of the three‑step elimination test cannot be overstated; it provides a systematic framework that empowers individuals to discern personal sensitivities. By maintaining a baseline log, one captures the nuanced variability inherent in daily dietary intake. The subsequent elimination week, though challenging, offers a clear demarcation of symptom trajectories. Re‑challenging with singular food groups isolates causative agents with precision. This iterative methodology not only informs dietary adjustments but also cultivates self‑awareness regarding gut‑brain interaction. Ultimately, the protocol bridges empirical observation with actionable change, fostering sustainable digestive health.
Maude Rosièere Laqueille
For anyone just starting out, I recommend focusing on hydration and keeping a simple food diary – it’s amazing how quickly patterns emerge.
Amanda Joseph
Sure, because a diary solves everything 🙄
Kevin Aniston
Remember, consistency is key; setting realistic portion goals and gradually introducing probiotic‑rich foods can transform your post‑meal experience. Celebrate each small victory, such as a day without noticeable swelling, to reinforce positive habits. If you encounter setbacks, review your log to pinpoint any hidden triggers you might have missed. Adjust your water intake accordingly – sometimes a mere half‑liter increase can make a substantial difference. Over time, you’ll develop an intuitive sense of what your gut tolerates, empowering you to make confident food choices without fear of discomfort.
kiran kumar
i knt even bllieve ppl still trust all these diet fads they are just a dsstraction from the real problem
Brian Johnson
Sounds like a solid plan – taking it step by step usually makes it less overwhelming.
Jessica Haggard
I appreciate the cultural angle; integrating familiar flavors makes the diet sustainable and enjoyable.
Alan Clark
Great stuff! Can’t wait to try the low‑FODMAP plan and see if it helps me feel lighter after meals.