Sulfonylurea Hypoglycemia Risk Calculator
Personalized Risk Assessment
Enter your age and kidney function to see which sulfonylurea has the lowest hypoglycemia risk for you.
Your Personalized Recommendation
Glyburide
High Risk
12.1 episodes/1,000 patient-years
Glimepiride
Moderate Risk
7.8 episodes/1,000 patient-years
Glipizide
Low Risk
4.2 episodes/1,000 patient-years
Why This Matters
Understanding your individual risk is crucial for safe diabetes management. Glyburide is associated with significantly higher hypoglycemia risk compared to other sulfonylureas, especially for:
- Adults over 65 years
- Patients with reduced kidney function (eGFR < 60)
- People with irregular eating patterns
The American Geriatrics Society specifically recommends avoiding glyburide in older adults. Glipizide is generally the safest option due to its short-acting nature.
When you're managing type 2 diabetes and your doctor suggests a sulfonylurea, it's easy to assume they're all the same. But they're not. The difference between one pill and another isn't just the name on the bottle-it’s the real, life-changing risk of low blood sugar. And that risk varies wildly depending on which sulfonylurea you take.
Why Sulfonylureas Still Matter
Sulfonylureas have been around since the 1950s, but they haven’t disappeared. In fact, in 2022, about 15% of U.S. adults with type 2 diabetes were still using them. Why? Because they work-and they’re cheap. Generic glipizide costs as little as $4 a month. Compare that to newer drugs like Ozempic, which can run over $500. For people on Medicare, Medicaid, or living in countries with limited healthcare access, sulfonylureas are often the only realistic option.They lower A1C by 1.5% to 2%, which is solid. But here’s the catch: they force your pancreas to keep releasing insulin, no matter what your blood sugar is doing. That’s why hypoglycemia-the dangerous drop in blood sugar-is their biggest problem.
Not All Sulfonylureas Are Created Equal
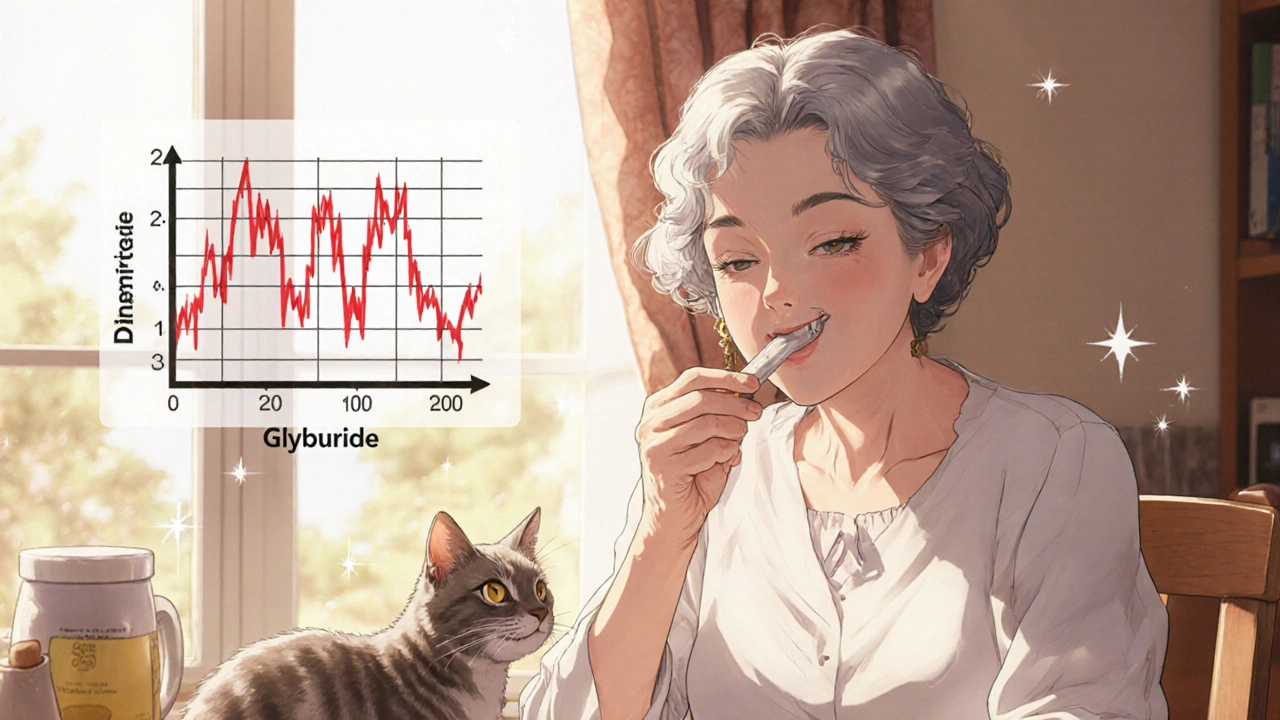
There are three main types you’ll hear about: glyburide, glimepiride, and glipizide. And their hypoglycemia risk? It’s not even close.Studies show glyburide (also called glibenclamide) is the worst offender. A 2017 study in Diabetes Care found people on glyburide had nearly three times the risk of severe hypoglycemia compared to those on glipizide or gliclazide. Why? Because glyburide sticks around too long. It has a half-life of 10 hours, and its metabolites can linger for up to 24 hours. That means even if you skip a meal or go for a walk after dinner, your body is still being flooded with insulin hours later.
Glimepiride is a step better, but still risky. It’s long-acting, too, and while it’s slightly more targeted to the pancreas than glyburide, it still carries a hypoglycemia rate of about 7.8 episodes per 1,000 patient-years.
Then there’s glipizide. This one’s different. It’s short-acting, with a half-life of just 2 to 4 hours. It kicks in fast, works for a few hours, and then clears out. That’s why it’s the preferred choice for older adults, people with irregular meals, or anyone at higher risk for lows. The 2019 American Journal of Managed Care analysis showed glipizide caused only 4.2 hypoglycemia episodes per 1,000 patient-years-less than half of glyburide’s 12.1.
Real People, Real Stories
Numbers tell part of the story. Real people tell the rest.On the American Diabetes Association’s online forum, one user, 'DiabetesWarrior42', wrote: ‘I was having 2-3 severe lows a month on glyburide. Since switching to glipizide, I’ve had zero.’ That’s not rare. In a thread of 87 people who switched, 63 reported fewer lows.
On Reddit, a user named 'Type2Survivor88' shared how he spent three days in the hospital at age 72 after his kidney function declined and his glyburide dose wasn’t adjusted. ‘My endocrinologist now says he never should have prescribed glyburide to someone my age,’ he wrote.
The FDA’s adverse event database confirms this pattern. Between 2018 and 2022, glyburide accounted for nearly 70% of all sulfonylurea-related hypoglycemia reports-even though it’s only prescribed about a third of the time.
Who Should Avoid Glyburide?
If you’re over 65, have kidney problems, or eat at unpredictable times, glyburide should be off the table.The American Geriatrics Society’s 2023 Beers Criteria explicitly says: Avoid glyburide in adults 65+. Why? Because older kidneys can’t clear it well. The active metabolites build up. And the longer the drug stays in your system, the more likely you are to crash-especially overnight, when you’re asleep and can’t eat.
Same goes for people with chronic kidney disease. The National Kidney Foundation says glyburide should be avoided if your eGFR is below 60. Glipizide? It’s safe until your eGFR drops below 30. That’s a huge difference.
Even if you’re younger and healthy, the risk isn’t zero. A 2021 meta-analysis found sulfonylureas carry 2.3 times the hypoglycemia risk of DPP-4 inhibitors and 3.7 times the risk of SGLT2 inhibitors. So if you have other options, glipizide is still the safest sulfonylurea.
What About Newer Forms?
There’s good news: glipizide just got better. In 2023, the FDA approved an extended-release version called Glucotrol XL. In clinical trials, it lowered hypoglycemia risk by 32% compared to regular glipizide. Why? Because it releases the drug slowly, avoiding those sharp insulin spikes. For people who still need a sulfonylurea but want smoother control, this is a real upgrade.
How to Use Sulfonylureas Safely
If you’re on a sulfonylurea, here’s what you need to do:- Start low. Glipizide usually begins at 2.5 mg. Glyburide at 1.25 mg. Never start high.
- Titrate slowly. Wait 2-3 weeks between dose changes. Your body needs time to adjust.
- Know the signs. Sweating, shaking, hunger, dizziness-these are early warning signs. Don’t wait until you’re confused or passing out.
- Use the 15-15 rule. If your blood sugar is below 70, take 15 grams of fast-acting sugar (juice, glucose tabs, candy), wait 15 minutes, check again. Repeat if needed.
- Talk to your doctor before hospitalization. Your dose should be cut in half if you’re admitted. Hospitals see 4.5 hypoglycemia episodes per 100 patient-years on sulfonylureas. That’s avoidable.
What’s the Bottom Line?
Sulfonylureas aren’t going away. But the days of treating them like interchangeable pills are over. Glyburide is a high-risk drug, especially for older adults and those with kidney issues. Glimepiride is better, but still carries a moderate risk. Glipizide-especially the new extended-release version-is the safest choice if you need a sulfonylurea.And if you’re on glyburide? Ask your doctor if switching to glipizide makes sense. Many people don’t realize they can get the same blood sugar control with far fewer lows. It’s not just about numbers on a screen-it’s about sleeping through the night without fear, driving without panic, and living without the constant shadow of a low.
Cost matters. But safety matters more. And when it comes to sulfonylureas, the cheapest pill isn’t always the best one.


Comments (14)
Hannah Machiorlete
Glipizide saved my life. I was on glyburide for two years and had three ER trips from lows. My grandma died from one. I switched last year and haven’t had a single episode. Why is this not common knowledge?
Bette Rivas
It’s critical to recognize that the pharmacokinetic profile of sulfonylureas directly correlates with hypoglycemia risk. Glyburide’s active metabolites-particularly 4-trans-hydroxyglyburide and 3-cis-hydroxyglyburide-have prolonged half-lives and retain full insulin-secretory activity. Glipizide, by contrast, undergoes rapid hepatic metabolism via CYP2C9 into inactive metabolites, minimizing accumulation. This is why guidelines from the ADA and AACE consistently recommend glipizide over glyburide in elderly patients and those with renal impairment. The data is robust and reproducible across multiple meta-analyses.
prasad gali
Let’s cut through the noise. Glyburide is a dinosaur. It’s like prescribing aspirin for a heart attack. The FDA data isn’t even close-70% of sulfonylurea-related hypoglycemia events? That’s not a side effect, that’s a systemic failure. If your provider still prescribes it to anyone over 60 or with eGFR <60, they’re either negligent or grossly uninformed. Glipizide ER is the new standard. Period.
Paige Basford
I love that you mentioned Glucotrol XL-I switched to it last month and honestly? I feel like I can breathe again. My glucose curve is so much smoother. I used to wake up at 3 a.m. sweating and terrified, but now I sleep through the night. I didn’t even know extended-release versions existed until I read this. Thank you for sharing this. I’m telling my whole family.
Ankita Sinha
This is such an important post! I’m a nurse in Delhi and we see so many patients on glyburide because it’s cheap and available. But I’ve seen so many elderly patients come in with confusion and seizures from hypoglycemia. I’ve started educating them on glipizide alternatives-even if it costs a bit more, it’s worth it. I wish more doctors here knew this. Can we get this translated into Hindi? I’d share it with my clinic.
Kenneth Meyer
There’s something deeply ironic about how we treat diabetes. We have drugs that can literally reverse the disease, yet we cling to 70-year-old pills because they’re cheap. Is it really about cost-or is it about who gets to be safe? The people on Medicaid, the elderly, the undocumented-they’re the ones getting the riskiest drugs. We call it ‘affordable care’ when it’s really just affordable risk.
Donald Sanchez
glipizide is the GOAT 🚀 i switched from glyburide and now i dont have to carry juice boxes everywhere. also glipizide xl is like magic beans 🌱 i used to get dizzy just walking to the fridge now im hiking on weekends. ps: my doc said 'i didnt know you could switch' lol
Abdula'aziz Muhammad Nasir
In Nigeria, we face the opposite problem: many patients never get any oral hypoglycemic at all. But when they do, glyburide is often the only option available due to supply chains. I agree with the science here-glipizide is superior. Perhaps international NGOs and pharmaceutical donors should prioritize distributing glipizide in low-resource settings. Safety should not be a luxury.
Tara Stelluti
Wait-so you’re telling me my doctor was trying to kill me? I’ve been on glyburide for 8 years. I had a seizure last Christmas. They said it was ‘just stress.’ Now I’m reading this and realizing… they didn’t even try to help. I’m switching tomorrow. And I’m telling everyone I know.
Danielle Mazur
Who benefits from glyburide being sold so cheaply? Big Pharma? The FDA? The insurance companies? Or is this all a calculated move to keep elderly patients dependent on emergency care? The numbers don’t lie-glyburide causes 70% of the hypoglycemia events. That’s not negligence. That’s a business model.
Margaret Wilson
Glipizide = freedom. 🎉 I used to live in fear of my own pancreas. Now I eat tacos at midnight and sleep like a baby. Who knew a $4 pill could give me back my life? Thank you for this post. I’m printing it and taping it to my doctor’s door.
william volcoff
Interesting that the extended-release glipizide reduces hypoglycemia by 32%. That’s not just a statistical win-it’s a quality-of-life revolution. But let’s not pretend this is the end of the story. We still need better alternatives. Sulfonylureas are a Band-Aid on a broken system. Still, if you’re stuck with one, glipizide XL is the only responsible choice.
Freddy Lopez
It’s easy to judge the past. Sulfonylureas were revolutionary in their time. But medicine evolves, and so must our practices. The real tragedy isn’t that glyburide exists-it’s that we still treat it as a default. Knowledge should be the cheapest drug of all. And yet, too many patients are still being prescribed based on inertia, not evidence.
Brad Samuels
I’m a type 2 diabetic and I’ve been on glipizide for five years. I never knew how much better I could feel until I read this. I used to think the lows were just part of the deal. Turns out, they weren’t. I feel like I’ve been living in grayscale and someone finally turned on the color. Thank you for writing this. I’m sharing it with my support group.